Women’s Heart Disease: Unique Symptoms and Risk Management

Heart disease kills more women than all forms of cancer combined. Yet, most women don’t realize it’s their biggest threat. In the U.S., about 307,000 women die from heart disease every year - that’s one in five. And here’s the problem: the symptoms don’t look like what you see in movies. No one clutches their chest and collapses dramatically. Instead, women get exhausted, nauseous, or feel like something’s just… off. And because doctors and patients alike expect the classic male pattern, women are often sent home with a diagnosis of anxiety or indigestion - even when their heart is failing.
What Women’s Heart Disease Actually Feels Like
The most common heart attack symptom for both men and women is chest discomfort. But for women, it rarely feels like a crushing weight. More often, it’s pressure - like a heavy band tightening around the ribs. Or it might not be chest pain at all. In fact, 43% of women who have heart attacks don’t have chest pain. That’s not rare. That’s the norm. Instead, women report symptoms that seem unrelated:- Unexplained fatigue so severe you can’t make your bed
- Shortness of breath while walking to the mailbox
- Jaw or back pain that comes and goes
- Nausea or vomiting with no stomach bug
- Dizziness or sudden lightheadedness
Why Women’s Hearts Are Different
Women’s hearts aren’t just smaller versions of men’s. They’re built differently. Women tend to have smaller coronary arteries. Their heart muscle responds differently to stress. Hormones play a role - especially after menopause, when estrogen drops. That’s when risk spikes. There are also conditions that mostly affect women:- Microvascular disease: Damage to the tiny arteries that feed the heart. It doesn’t show up on standard angiograms. Symptoms? Fatigue, shortness of breath, and chest tightness during activity - not rest.
- SCAD (Spontaneous Coronary Artery Dissection): A tear in a heart artery with no warning. It’s the leading cause of heart attacks in women under 50, especially during or after pregnancy.
- Takotsubo cardiomyopathy (also called broken heart syndrome): Triggered by extreme emotional or physical stress. The heart temporarily enlarges and doesn’t pump well. It looks like a heart attack, but there’s no blocked artery.
The Silent Killer: Silent Heart Attacks
Some heart attacks don’t hurt. They’re silent. And women over 65 are 34% more likely than men to have one without knowing it. No pain. No warning. Just unexplained fatigue, nausea, or a sudden drop in energy. A woman in her 70s in Edmonton thought she was just getting older. She stopped gardening. She slept more. Her family assumed it was normal aging. Six months later, she collapsed. An EKG showed she’d had three silent heart attacks - all in the past year. Silent heart attacks aren’t less dangerous. They’re more dangerous. Because you don’t know you’re in trouble, you don’t get treatment. And each one weakens your heart further.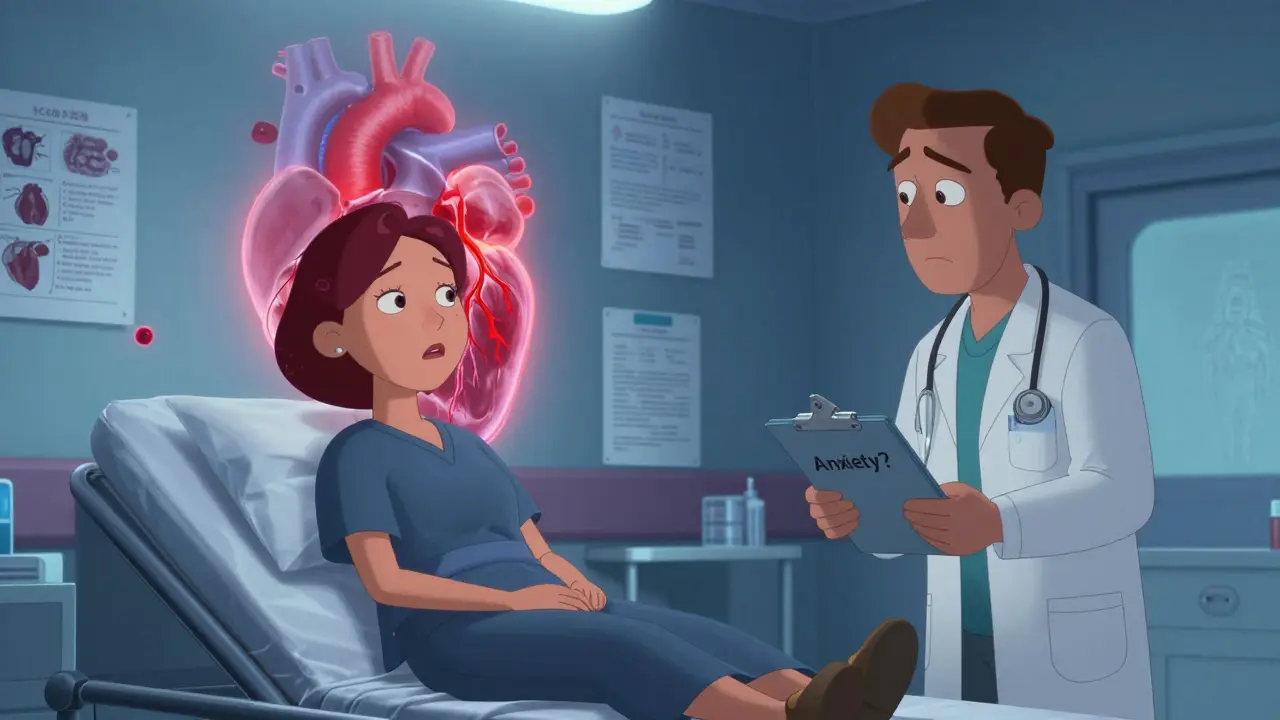
What Makes Women More at Risk
Some risks are the same as for men - smoking, high blood pressure, obesity, diabetes. But women have unique triggers:- Pregnancy complications: Preeclampsia, gestational diabetes, or giving birth prematurely can double or even triple your risk of heart disease later.
- Early menopause: Losing estrogen before 45 raises risk significantly.
- Autoimmune diseases: Lupus and rheumatoid arthritis inflame blood vessels and damage the heart.
- Chronic stress: Women are 37% more likely than men to have angina triggered by emotional stress - not physical exertion.
- Depression and anxiety: These aren’t just mental health issues. They’re heart disease risk factors, especially in women.
How to Protect Yourself
You can’t change your genes. But you can change your habits. Here’s what works:- Track your menstrual and pregnancy history: If you had preeclampsia, gestational diabetes, or early menopause, tell your doctor. That’s not just history - it’s your future risk profile.
- Know your numbers: Blood pressure, cholesterol, and blood sugar matter. Aim for under 120/80, LDL under 100, and fasting glucose under 100.
- Move every day: 30 minutes of brisk walking five days a week cuts heart disease risk by 30%. It doesn’t have to be intense. Just consistent.
- Manage stress: Try breathing exercises, yoga, or just 10 minutes of quiet each morning. Chronic stress is a silent heart killer.
- Don’t ignore fatigue: If you’re exhausted for more than two weeks - and it’s not just sleep deprivation - get checked. It’s the most common warning sign.

What to Ask Your Doctor
Most doctors aren’t trained to look for women’s heart disease. You have to lead the conversation. Here’s what to say:- “I’ve been unusually tired for weeks. Could this be heart-related?”
- “I have jaw pain that comes and goes. Should I get tested for microvascular disease?”
- “I had preeclampsia during pregnancy. What’s my risk now?”
- “Can you check for SCAD if I’ve had unexplained chest tightness?”
- “Is there a test that works better for women than a standard stress test?”
Where to Get Help
There are now 147 certified Women’s Cardiovascular Centers of Excellence across the U.S. These hospitals have protocols specifically designed for women. They know to test for microvascular disease. They don’t dismiss fatigue. They understand SCAD. If you’re in Canada, ask your doctor about the RENEW initiative - a $150 million federal research program launched in 2023 focused on women’s heart health. Many Canadian hospitals are now part of this network. And if you’re not sure where to start, visit WomenHeart or the American Heart Association’s Go Red for Women site. They offer free symptom checklists, doctor question guides, and local support groups.It’s Not Too Late
You don’t need to be perfect. You just need to be aware. Heart disease isn’t inevitable. It’s preventable - if you know the signs. A woman in her 60s in Calgary started tracking her energy levels after reading about ‘vital fatigue.’ She noticed she couldn’t carry groceries anymore without stopping. She went to her doctor. They did a Corus CAD test. It showed early blockages. She started medication, changed her diet, and walked daily. Two years later, she’s hiking with her grandkids. Your heart doesn’t care if you’re a mom, a grandmother, a professional, or a retiree. It just needs you to listen. Don’t wait for the chest pain. Listen to the fatigue. The nausea. The jaw pain. The breathlessness. Those are your heart speaking.Do women have different heart attack symptoms than men?
Yes. While chest pain is common in both, women are more likely to have symptoms like extreme fatigue, shortness of breath, nausea, jaw or back pain, and dizziness - often without chest discomfort. About 43% of women who have heart attacks don’t feel chest pain at all. These symptoms are easily mistaken for stress, anxiety, or aging, which delays treatment.
Is heart disease really the #1 killer of women?
Yes. Heart disease kills about 1 in 5 women in the U.S. each year - more than all cancers combined. Globally, it causes 8.9 million female deaths annually. Yet, only 44% of women recognize it as their leading cause of death, partly because symptoms are different and less visible than in men.
Can stress cause a heart attack in women?
Yes. Mental stress triggers angina and heart attacks in women 37% more often than in men. Emotional shock, grief, or chronic anxiety can cause Takotsubo cardiomyopathy - a condition where the heart temporarily weakens, mimicking a heart attack. This is why emotional health is part of heart health for women.
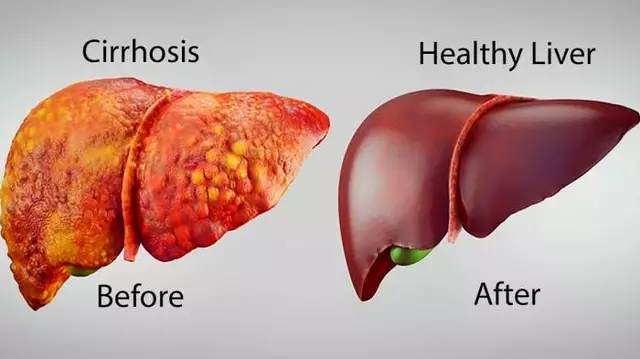
What is microvascular disease and why does it affect women more?
Microvascular disease affects the tiny arteries that feed the heart muscle, not the large ones seen in typical blockages. It’s more common in women, especially after menopause, due to hormonal changes and smaller artery size. Symptoms include fatigue, shortness of breath, and chest tightness during activity - not rest. Standard heart tests often miss it, so specialized tests like the Corus CAD blood test are needed.
Should I get tested for heart disease if I have no symptoms?
If you have risk factors - like a history of preeclampsia, early menopause, diabetes, or autoimmune disease - yes. Silent heart attacks are common in women over 65. If you’ve had unexplained fatigue, shortness of breath, or nausea for more than two weeks, get checked. Prevention isn’t just for people with symptoms. It’s for anyone who wants to stay healthy.
Are there tests that work better for women?
Yes. The Corus CAD test analyzes gene expression to detect coronary artery disease in women with 88% accuracy - much better than traditional stress tests, which miss up to 40% of cases in women. Other tools like cardiac MRI and CT angiography are also more effective for detecting microvascular disease. Ask your doctor if these are right for you, especially if you have symptoms but normal stress test results.





Elizabeth Cannon
January 23, 2026 AT 14:22omg i thought i was just getting old or stressed but last year i was so tired i couldnt even fold laundry and my jaw hurt for weeks-doc said anxiety. turned out i had microvascular disease. why dont they teach this in med school??
Phil Maxwell
January 23, 2026 AT 22:37that calgary woman’s story hit me hard. my mom had the exact same thing-thought it was menopause. she’s fine now but it took three ER visits. why is this still not common knowledge?
Shelby Marcel
January 25, 2026 AT 17:15i had a silent heart attack in my 50s and never knew. just felt like i’d been hit by a bus for a week. got lucky my sister insisted on bloodwork. this needs to be on every women’s health checklist.
Don Foster
January 26, 2026 AT 21:39the corus cad test is the only thing that matters stop wasting time on stress tests theyre 40 percent useless for women and everyone knows it but hospitals still use them because its cheaper and easier
Izzy Hadala
January 27, 2026 AT 18:38While the epidemiological data presented is compelling and aligns with contemporary cardiovascular research, the absence of standardized diagnostic protocols across regional healthcare systems remains a critical barrier to equitable outcomes. The disproportionate misdiagnosis rate among women, particularly in emergency settings, reflects a systemic failure in clinical training rather than a deficiency in patient awareness. Further longitudinal studies are required to quantify the efficacy of gender-specific interventions such as the RENEW initiative and to establish biomarker thresholds for microvascular dysfunction independent of traditional angiographic criteria.
Patrick Gornik
January 28, 2026 AT 11:59let’s be real-the medical industrial complex doesn’t want you to know your heart can scream without a single scream. they profit off the slow rot of misdiagnosed women. microvascular disease? SCAD? takotsubo? these aren’t conditions-they’re inconvenient truths that don’t fit the 1950s male model of cardiac suffering. we’ve turned the female body into a glitch in the algorithm. and now we’re surprised when it crashes?
siva lingam
January 30, 2026 AT 05:27so women die more from heart disease… and the solution is to ask your doctor more questions? wow. revolutionary. next up: water is wet and gravity exists
Marlon Mentolaroc
January 31, 2026 AT 03:06lol i work in ER and we see this every week. women come in saying they’re exhausted and we give them antacids. one lady told me she couldn’t lift her coffee cup-turned out her LAD was 95% blocked. we’re not evil, we’re just trained to look for the textbook. but yeah… we’re failing.
Gina Beard
February 1, 2026 AT 15:11awareness is not action. knowing is not healing.
blackbelt security
February 3, 2026 AT 11:43if you’re tired for two weeks-get checked. no excuses. your heart doesn’t care if you’re busy. it just needs you to listen. walk. eat clean. ask for the corus test. save yourself.
Tommy Sandri
February 4, 2026 AT 19:38in many cultures, women are socialized to prioritize others’ needs above their own. this behavioral norm compounds biological risk factors. the true epidemic is not just medical-it’s cultural. we must reframe women’s health as a societal imperative, not an individual burden.