Post-thrombotic syndrome: what it is and what to do now
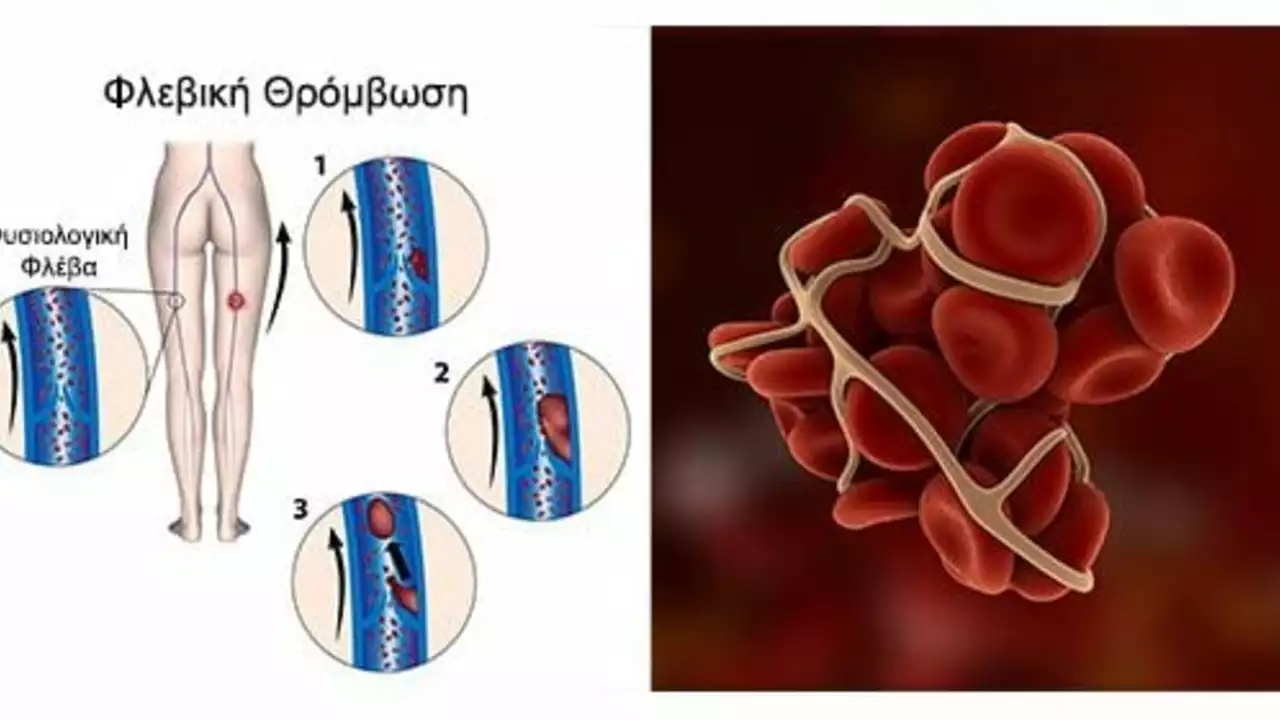
About one in three people who get a deep vein thrombosis (DVT) end up with post-thrombotic syndrome (PTS). PTS is long-term damage to leg veins after a clot. It shows up as pain, swelling, skin darkening, and sometimes ulcers. You don't need fancy tests to start helping yourself - practical steps often make the biggest difference.
PTS usually appears months after a DVT but can show up years later. The problem is damaged valves inside the veins and scarring that makes blood pool in the leg. Blood pooling raises pressure in the veins and tissues, causing aching, heaviness, and that tight, tired feeling. Symptoms often get worse after standing or walking and improve with leg elevation.
Symptoms and diagnosis
Look for persistent swelling, aching, itching, skin changes, or hardening of the leg tissue. Dark brown patches near the ankle and slow-healing wounds are warning signs of severe PTS. Your doctor will review your history, exam the leg, and usually do a duplex ultrasound to check for vein reflux or residual clot. Diagnosis is mostly clinical - the scan helps plan treatment but doesn't always explain how you feel.
Treatment and prevention
Compression stockings are the mainstay: they lower vein pressure, reduce swelling, and ease pain. Start with a proper fitting; graduated compression (20-30 mmHg or stronger if advised) works best. Daily walking and calf exercises improve calf muscle pump function and help push blood back to the heart. Elevate the leg when resting and avoid long periods of sitting or standing.
Good wound care matters if you have skin breakdown. Clean the area, keep pressure off the wound, and see a wound clinic if it doesn't improve in a week or two. Your doctor may recommend topical dressings, debridement, or referral to a vascular specialist. For ongoing clot risk, follow anticoagulation advice - proper blood thinner use after DVT lowers the chance of worse PTS.
In some cases, procedures can help. Angioplasty, stenting, or catheter-directed thrombectomy can open blocked or scarred veins for selected patients with severe symptoms. These are not routine steps; they are considered when conservative measures fail and imaging shows treatable blockages.
Simple lifestyle changes add measurable benefits: lose extra weight, quit smoking, control blood pressure, and treat varicose veins if advised. If you have a recent DVT, ask your clinician about early compression and structured exercise to reduce PTS risk.
If your leg pain, swelling, or skin changes are new or getting worse, see a clinician. Timely care reduces complications, speeds recovery, and lowers the chance of ulcers. You don't have to accept chronic leg pain - there are practical options that help most people feel better.
Practical daily tips: wear loose clothes that don't squeeze the thigh, change socks when they get tight, massage gently toward the heart if recommended, and stay hydrated. Track symptoms with photos and notes so you can show your doctor changes over time. If leg ulcers or severe pain limit walking, ask about referral to a vascular clinic - quicker assessment can prevent lifelong problems.
Start today.
Post-Thrombotic Syndrome: A Common Complication of Deep Vein Thrombosis
Well, folks, here we go! Post-Thrombotic Syndrome, or as I like to call it, "the annoying aftermath of Deep Vein Thrombosis." It's like that one guest who just doesn't know when to leave the party. Essentially, it's a common complication that may follow a bout of Deep Vein Thrombosis (DVT). It's a tricky little number, causing symptoms like pain, swelling, and skin changes in the affected limb. So, if you've had DVT, keep an eye out for this persistent party crasher!
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



