Post-Thrombotic Syndrome: A Common Complication of Deep Vein Thrombosis
A Brief Introduction to Post-Thrombotic Syndrome
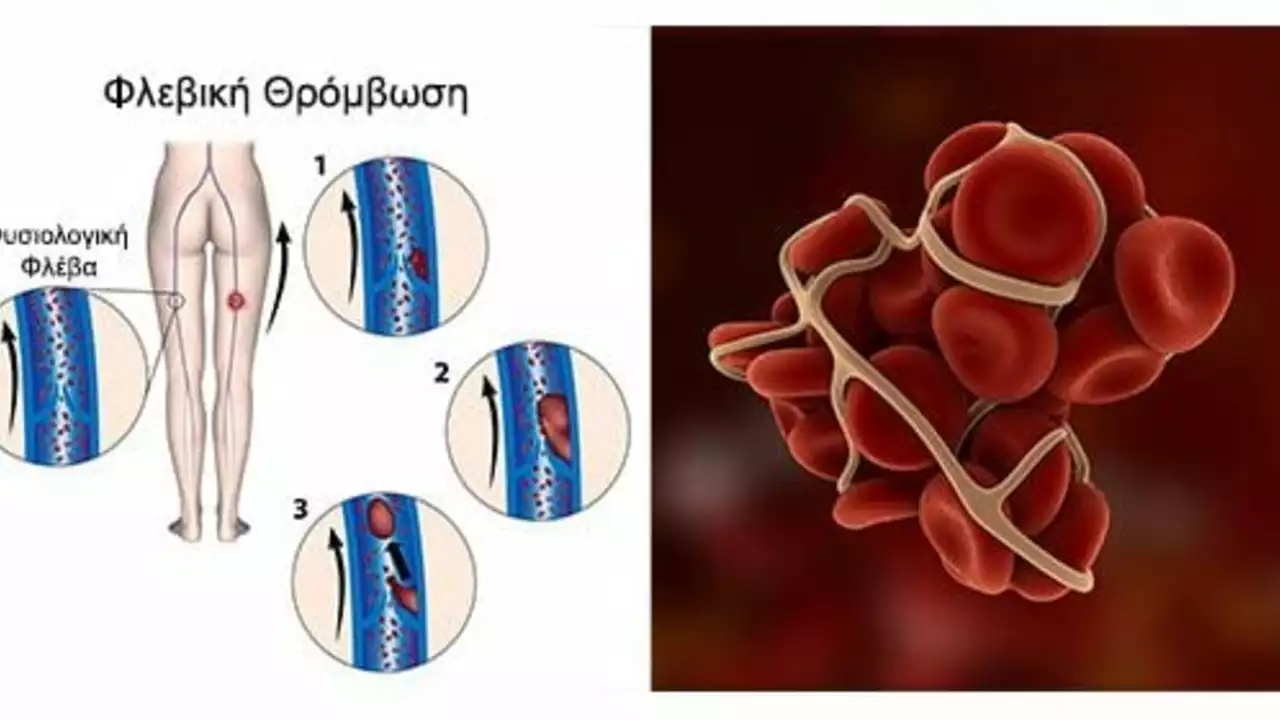
Some years back, I got pretty sick and ended up having Deep Vein Thrombosis (DVT). Whoa, big word drop right? Let me break that down. Deep Vein Thrombosis is basically a blood clot that forms in a deep vein, usually in the leg. But hold on, here's where it gets interesting, and by interesting, I mean scary. This seemingly harmless blob of clot can go rogue, catch the next expressway on your blood's flow and lodge itself in your lungs, causing a pulmonary embolism. Now, that's a party you don't want to crash!
Anyway, where was I? Oh yes, I was telling you about my uncanny encounter with DVT. Well, what came next was something I didn’t see coming, something called Post-Thrombotic Syndrome (PTS). Now, that's a whole other level of thrombotic tomfoolery! So, sit back, grab a cup of coffee, and let's delve into this critical matter with the gusto of my Labrador, Baxter, hunting for his favorite chew toy.
Understanding the Ins and Outs of Post-Thrombotic Syndrome
As someone who's been through the murky waters of PTS, let me tell you, it's not a cup of tea. Imagine you're trying to climb a hill, but your legs feel like they're filled with lead, and they're always swollen, like the time Baxter got stung by a bee. Add a little dash of skin discoloration and recurrent ulcers, and voila, you've got Post-Thrombotic Syndrome.
Painful right? That's because the blood clots from DVT can damage the veins and disrupt the blood flow from the legs to the heart. It is a common complication of DVT, affecting nearly half of the patients. And, unlike my little Vivienne's ballet performances, it’s not something to look forward to.
How to Identify the Signs and Symptoms
I remember the first time I noticed my symptoms of PTS, I was walking Lachlan, my son, to the school bus, and I felt an uncharacteristic heaviness and swelling in my legs. I knew then that something was amiss.
This can be experienced differently by different individuals – kind of like how everyone experiences Monday blues differently. Some common symptoms include swelling of the legs, redness and scaling, and even ulcers in severe cases. Hey, I told you this wasn't a fun ride to join
Unveiling the Risk Factors
Risk factors for PTS? Now, that's a topic as broad as the ocean. And trust me, my friends, I've sailed those waves. For starters, having a history of DVT itself puts you at risk. Also, immobility, obesity, age, the severity of initial DVT all come into play.
Basically, anything that increases your chances of DVT consequently increases your chances of developing PTS. As the famous saying goes, where one trouble goes, the other follow – like annoying siblings, you can't separate them.
Preventing the Unpreventable: Can we really?
Now, on to the question that is probably running in your minds: Can we really prevent PTS? I wish the answer were as straightforward as my kids' math homework. But alas, it takes a bit more thinking.
While you can't entirely prevent PTS, there are many ways to reduce the risk. It's all about managing your DVT and staying ahead of your game, like anticipating where Baxter might hide the TV remote. Anticoagulant therapy, compression stockings, or simply regular check-ups can go a long way.
The Silver Lining: Treatment Options
The good news is, like every dark cloud, there's a silver lining for PTS too. There are treatments available, from medication to physical therapy to surgical interventions. So fear not, as others before you, like yours truly, have braved the storm and come out the other end, maybe not unscathed, but definitely triumphant.
Managing PTS is all about managing symptoms and preventing further complications. You can liken it to managing a toddler throwing tantrums - it's all about patience, persistence, and finding the right approach.
Sewing it up: Be your own Health Advocate
The journey with PTS has been quite a roller coaster ride! From the highs of getting better to the lows of managing symptoms and treatment, it's been both daunting and enlightening. But if there is one thing that I learned from this journey, it's the importance of being your own health advocate.
Whether it's asking your doctor a million questions, or donning those oh-so-sexy compression stockings and strolling around the house, it's all in your hands. A dash of positivity, a sprinkle of perseverance, a spoonful of patience, and a whole lot of resilience – that's the recipe for managing PTS, folks!





chuck thomas
August 1, 2023 AT 17:16Reading through your experience with post‑thrombotic syndrome feels like traveling a rugged trail while carrying a lantern. The way you described the heaviness in your legs really captures the physiological burden that many patients overlook. It's a reminder that early DVT management can spare us from a cascade of chronic complications. Keep sharing these stories-they light the way for others navigating the same storm. Stay strong, and keep that Labrador spirit alive.
Gareth Pugh
August 6, 2023 AT 14:30Deep veins, hidden dangers. Clots linger, veins mourn. Compression stockings become silent heroes.
Illiana Durbin
August 11, 2023 AT 11:43Your resilience shines through every line.
Tyler Heafner
August 16, 2023 AT 08:56I commend the thoroughness of your account. The clinical details are presented with due gravity, which aids comprehension. Moreover, emphasizing patient advocacy aligns with best practice standards. Your narrative sets a valuable precedent for others facing similar health hurdles.
anshu vijaywergiya
August 21, 2023 AT 06:10Oh, the drama of swollen legs! Your tale paints a vivid tapestry of pain, perseverance, and the occasional triumph. When you speak of Baxter’s relentless spirit, it feels like a rallying cry for all of us battling PTS. Remember, every step you take, however tentative, is a victory against the lingering shadow of DVT. Let the world hear your roar, and may your compression stockings be as bold as your resolve.
ADam Hargrave
August 26, 2023 AT 03:23Ah, the “great” American medical system-always ready with a pamphlet that reads like a bedtime story. 😏 But seriously, if you can’t get a proper follow‑up, you might as well try juggling flaming torches. At least the emojis keep us entertained while we wait for real solutions. Keep fighting the good fight, and maybe one day the paperwork will give way to actual care.
Michael Daun
August 31, 2023 AT 00:36hey man thx 4 sharing this u rock i think compression is key u know its like a hug for your veins its cheap and works well also watch ur weight it helps alot keep up the good work
Rohit Poroli
September 4, 2023 AT 21:50From a physiotherapy perspective, the venous return impairment described underscores the need for early mobilization protocols. Integrating graduated compression therapy with duplex ultrasound monitoring can mitigate ulcerogenesis. Moreover, leveraging patient‑centered education reduces non‑adherence rates dramatically. Your narrative provides a solid case study for interdisciplinary care pathways.
William Goodwin
September 9, 2023 AT 19:03Bravo on turning a medical saga into a captivating saga! 🌟 Your vivid analogies make the pathology feel less like a textbook and more like an adventure. The way you compare compression stockings to a superhero cape is pure gold. Keep sprinkling those emojis-you’re making the science sparkle! 🚀
Isha Bansal
September 14, 2023 AT 16:16Post‑thrombotic syndrome, often abbreviated as PTS, represents a chronic sequela that follows an acute deep vein thrombosis event, lingering long after the initial clot has resolved; its pathophysiology involves venous valvular damage, persistent hypertension, and inflammatory remodeling of the vein wall. Patients frequently describe a sensation of heaviness, reminiscent of carrying a sack of bricks, accompanied by intermittent swelling that fluctuates with activity and elevation. The skin may acquire a reddish or brownish hue, a tell‑tale sign of hemosiderin deposition, while chronic venous ulcers can develop in the most severe cases, posing a significant wound‑care challenge. Epidemiological data suggest that up to half of individuals who survive a DVT will eventually manifest some form of PTS, underscoring the public health relevance of this condition. Early initiation of anticoagulation, coupled with timely compression therapy, has been shown in multiple randomized trials to reduce the incidence and severity of PTS. Moreover, patient education regarding leg elevation, regular ambulation, and weight management plays a pivotal role in mitigating venous stasis. The use of graduated compression stockings, typically exerting 30–40 mmHg at the ankle, improves calf muscle pump efficiency and alleviates edema. Lifestyle modifications, such as avoidance of prolonged immobility during travel and adherence to physiotherapy regimens, further support venous return. In refractory cases, interventional procedures like venous angioplasty, stenting, or surgical venous bypass may be considered, though these carry their own risk profiles. It is essential for clinicians to adopt a multidisciplinary approach, engaging vascular surgeons, wound care specialists, and physical therapists in the management plan. Regular follow‑up visits enable the monitoring of symptom progression and the early detection of complications, such as cellulitis or new ulcer formation. While pharmacologic options remain limited, emerging therapies targeting inflammatory pathways hold promise for future intervention. Patient advocacy groups also provide valuable resources, fostering community support and sharing of practical coping strategies. Ultimately, the goal of treatment is not merely symptom control but the preservation of quality of life and functional independence. By maintaining vigilance and employing evidence‑based strategies, the medical community can significantly blunt the impact of PTS on millions of patients worldwide.
Ken Elelegwu
September 19, 2023 AT 13:30While your exposition is undeniably exhaustive, one might argue that the practical take‑aways could be distilled into a more succinct checklist. Nevertheless, the academic rigor displayed is commendable, and the readers will surely appreciate the depth.
Gene Nilsson
September 24, 2023 AT 10:43It is with great respect that I address the complexity of post‑thrombotic syndrome. The presented data aligns with current clinical guidlines, however, some clarifications are warranted. Please ensure that the compression stocking gradient is percribed correctly. Your dedication to patient eduaction is laudable.
Vintage Ireland
September 29, 2023 AT 07:56Absolutely spot on-those little details can make all the difference. Keep up the good work, and thanks for pointing that out!
Anshul Gupta
October 4, 2023 AT 05:10Another bland recount of PTS-nothing new, just the same old spiel. Guess we’ll see if anyone actually reads this.