Understanding Mast Cells: Role, Triggers, and Health Effects
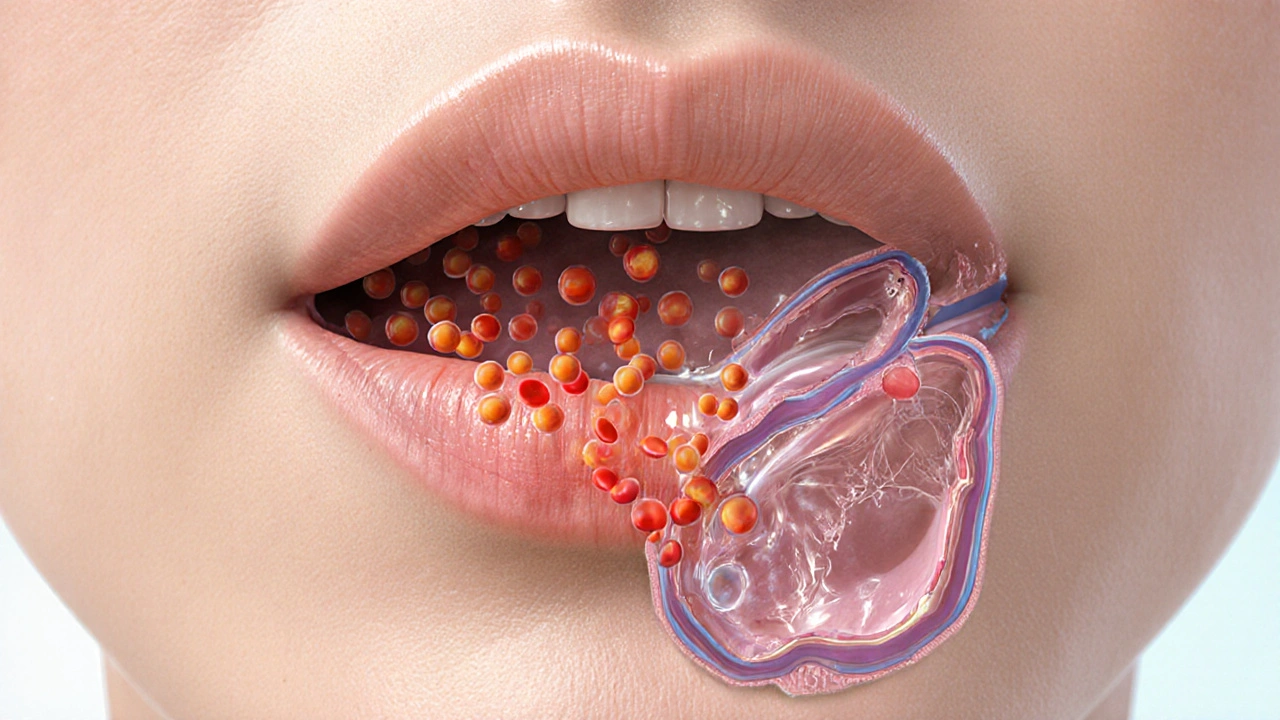
When working with mast cells, immune cells that store and release mediators like histamine. Also known as granulocytes, they sit in skin, lungs, and gut, ready to react when something goes wrong. Histamine is the primary chemical they dump, causing itching, swelling, and the classic runny nose. Because they sit at the front line of the immune system, mast cells link everyday irritants to full‑blown allergic reactions. In short, mast cells detect a threat, release histamine, and trigger inflammation – a three‑step chain that keeps us safe but can also cause discomfort when the alarm is too loud.
One major player that works hand‑in‑hand with mast cells is inflammation. When mast cells release their payload, blood vessels widen, fluid leaks into tissues, and immune cells swarm the area. That response is essential for fighting wounds, yet when it sticks around for too long it fuels chronic conditions like eczema or asthma. Another key factor is the type of trigger: food allergens, pollen, insect venom, or even stress can set mast cells off. The sensitivity varies by person, which is why some folks sneeze at a hint of perfume while others only react to a bee sting. Understanding these triggers helps you pick the right antihistamine or lifestyle tweak to keep the reaction in check.
What You’ll Find Below
Below this quick rundown, you’ll discover a curated set of articles that dive deeper into how mast cells intersect with everyday health topics. From detailed guides on buying generic medications online to practical tips for managing skin inflammation, each post connects back to the core idea that mast cells and their mediators shape many of the symptoms we talk about. Whether you’re looking for safe ways to purchase an allergy drug or want to learn how Tai Chi can soothe gut inflammation, the collection gives you actionable insights backed by clear explanations.
How Histamine Triggers Angioedema: Causes, Symptoms, and Treatment
Learn how histamine triggers angioedema, how to spot it, and the best treatments. Get clear differences from bradykinin‑mediated swelling and practical prevention tips.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



