How Histamine Triggers Angioedema: Causes, Symptoms, and Treatment
Histamine Angioedema Symptom Checker
Answer the following questions to determine if your swelling is likely histamine-mediated and what treatment options may be effective.
Click "Check My Symptoms" to see if your symptoms suggest histamine-mediated angioedema.
When swelling shows up suddenly on the lips, tongue, or eyes, many people think of an allergic reaction. The real culprit is often histamine, a molecule that can make blood vessels leak and tissues swell within minutes. Understanding why this happens, how it differs from other forms of angioedema, and what you can do about it turns a scary episode into a manageable condition.
TL;DR
- Histamine is released from mast cells and basophils during allergic reactions.
- It binds to H1 and H2 receptors, causing blood‑vessel dilation and fluid leakage that leads to angioedema.
- Bradykinin‑mediated angioedema looks similar but does not respond to antihistamines.
- Rapid treatment with antihistamines, corticosteroids, or epinephrine can stop histamine‑driven swelling.
- Identify triggers (foods, drugs, insect bites) and carry emergency medication if you’ve had episodes before.
What Is Histamine?
Histamine is a biogenic amine that regulates immune responses, gastric acid secretion, and neurotransmission. In the immune system, it sits in granules inside mast cells and basophils, waiting for a signal to spill out. When an allergen crosses‑links IgE antibodies on a mast cell’s surface, the cell tears open and dumps histamine into nearby tissue.
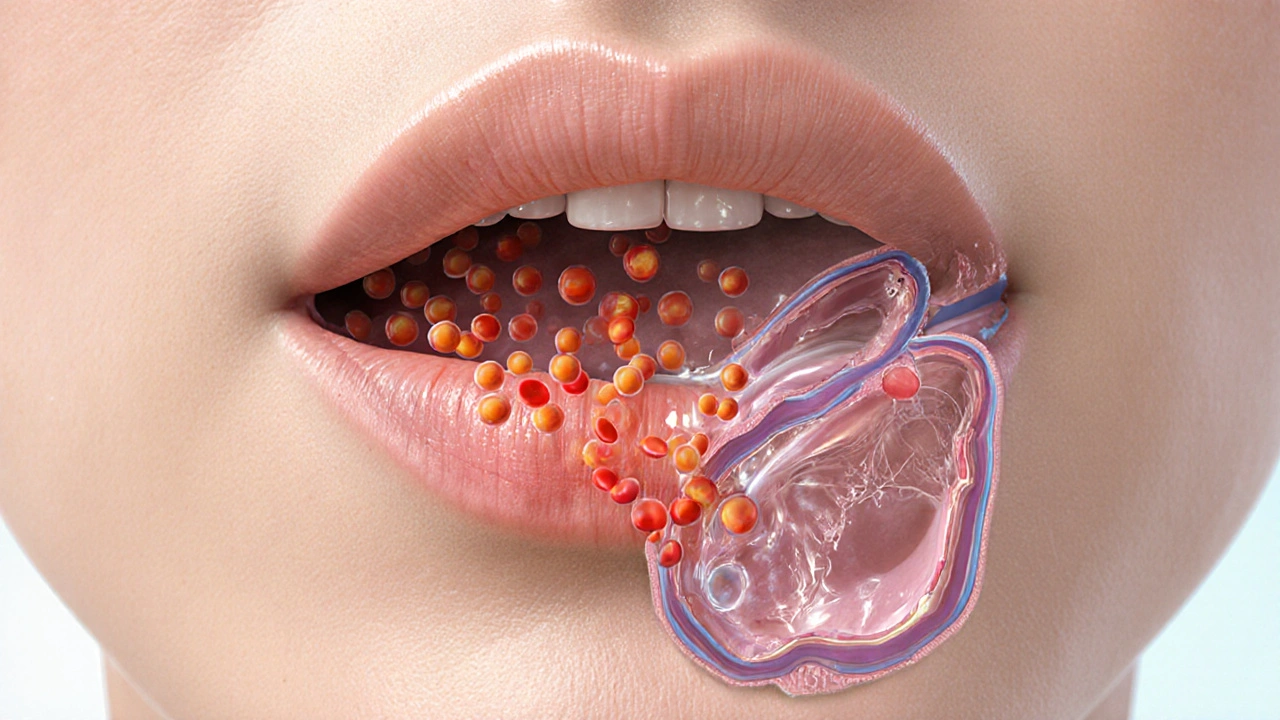
Once in the extracellular space, histamine attaches to receptors on blood‑vessel walls, nerves, and smooth muscle. The most relevant for swelling are the H1 and H2 receptors, which trigger a cascade that loosens the tight junctions between endothelial cells. The result: fluid leaks into the surrounding tissue, producing the hallmark puffiness of angioedema.
How Histamine Causes Angioedema
Mast cells are immune sentinels located in skin, mucosa, and around blood vessels. Their primary role is to release inflammatory mediators like histamine when they sense a threat. When an allergen binds to IgE on a mast cell, a rapid degranulation event occurs, releasing histamine within seconds.
The H1 receptor, found on endothelial cells and sensory nerves, causes two key effects: (1) vasodilation, which raises blood flow to the area, and (2) increased vascular permeability, allowing plasma proteins and fluid to seep out. This extracellular fluid accumulates in the loose connective tissue of the lips, eyelids, and oral cavity, creating the deep, non‑pitting swelling we call angioedema.
H2 receptors, while best known for stimulating stomach acid, also reside on blood‑vessel smooth muscle. Their activation augments the H1‑mediated leak, especially in the gastrointestinal tract where histamine‑driven angioedema can present as abdominal pain and vomiting.
Other Pathways: Bradykinin and the Complement System
Not all angioedema is histamine‑driven. Bradykinin is a peptide that increases vascular permeability through a separate receptor (B2) and is the main player in hereditary and ACE‑inhibitor‑induced angioedema. Because bradykinin does not activate H1/H2 receptors, antihistamines and steroids are usually ineffective.
The complement cascade can also generate C2‑kallikrein, which produces bradykinin. IgE mediated reactions tend to be histamine‑heavy, whereas IgG or IgM immune complexes can trigger complement‑driven swelling. Differentiating these pathways matters for treatment choice.
For patients on ACE inhibitors, the enzyme that normally breaks down bradykinin is blocked, allowing the peptide to accumulate and cause sudden facial swelling that does not respond to traditional allergy meds.
Spotting Histamine‑Mediated Angioedema
Typical signs include:
- Rapid onset (minutes to a couple of hours) after exposure to a known trigger.
- Swelling of lips, tongue, eyelids, or genital area without the raised, red rash seen in urticaria.
- Accompanying itching, burning, or tingling sensations.
- Potential involvement of the airway-tightening of the throat or voice changes.
Common triggers are foods (nuts, shellfish), insect stings, latex, certain medications (NSAIDs, penicillins), and physical factors like temperature changes.
Because histamine also affects nerves, patients may feel a prickly or “ants‑in‑the‑skin” sensation before the swelling becomes obvious.

Managing Histamine‑Driven Angioedema
The frontline drugs target the H1 receptor:
- Second‑generation antihistamines (cetirizine, loratadine, fexofenadine) provide relief without drowsiness and are safe for most adults.
- First‑generation agents (diphenhydramine) work quickly but cause sedation; they’re useful for acute episodes.
Corticosteroids (prednisone) help reduce the inflammatory cascade and prevent late‑phase swelling that can linger after histamine levels drop.
In severe cases where airway compromise is possible, epinephrine is the drug of choice. It constricts blood vessels, relaxes airway muscles, and reverses histamine’s effects within minutes. Carry an auto‑injector if you’ve experienced life‑threatening swelling.
For patients with recurrent episodes, a daily prophylactic antihistamine can keep mast cells from over‑reacting, especially during allergy seasons.
Prevention Strategies
Identify and avoid known allergens. A detailed diary of foods, medications, and environmental exposures can reveal patterns. Skin‑prick testing or specific IgE blood tests help confirm suspicions.
For drug‑related angioedema, discuss alternatives with your physician. If you’re on an ACE inhibitor and have experienced swelling, switching to an ARB (angiotensin‑II receptor blocker) often eliminates the risk.
Maintaining a healthy gut microbiome supports the immune system and may lower baseline mast‑cell activity. Probiotic‑rich foods, regular exercise, and stress‑management techniques are simple daily habits.
When to Seek Emergency Care
If swelling involves the tongue, floor of the mouth, or throat and you feel difficulty breathing, speak, or swallow, call emergency services immediately. Even with a known history, airway obstruction can progress rapidly.
Additional red‑flag signs include:
- Rapid progression of swelling within minutes.
- Hoarseness or a “tight” feeling in the throat.
- Hives or widespread rash appearing alongside swelling.
- Drop in blood pressure or fainting.
Prompt epinephrine administration followed by transport to an emergency department is the safest approach.
Quick Comparison: Histamine vs. Bradykinin Angioedema
| Feature | Histamine‑Mediated | Bradykinin‑Mediated |
|---|---|---|
| Typical Triggers | Allergens, drugs (NSAIDs), insect bites | ACE inhibitors, hereditary C1‑esterase deficiency |
| Response to Antihistamines | Usually rapid improvement | Little to none |
| Onset | Minutes to 2hours after exposure | 30minutes to several hours |
| Associated Symptoms | Itching, erythema, hives may accompany | Often no itch; may have abdominal pain |
| Treatment of Choice | Antihistamines ± corticosteroids ± epinephrine | C1‑esterase inhibitor, icatibant, or stopping ACE‑I |
Key Takeaways
Histamine is the primary driver behind most acute angioedema episodes linked to allergies. Recognizing the fast‑acting nature of H1/H2 receptor activation helps you choose the right rescue meds-antihistamines, steroids, and epinephrine. Distinguishing histamine‑driven swelling from bradykinin‑mediated forms is critical because the latter won’t respond to typical allergy drugs and requires different therapies.
Stay proactive: keep a symptom diary, avoid known triggers, and carry an epinephrine auto‑injector if your doctor recommends one. With the right knowledge, you can turn a frightening flare‑up into a manageable event.
Frequently Asked Questions
Can antihistamines cure angioedema?
Antihistamines work well for histamine‑mediated angioedema, especially when taken early. They won’t help with bradykinin‑driven swelling, which requires specific inhibitors or stopping the triggering medication.
Why does ACE‑inhibitor angioedema not respond to allergy meds?
ACE inhibitors block the breakdown of bradykinin, leading to its buildup. Since bradykinin acts on a different receptor (B2), antihistamines and steroids have little effect. The solution is to discontinue the ACE inhibitor and consider a bradykinin‑targeted drug if swelling is severe.
Is it safe to use diphenhydramine for an acute episode?
Diphenhydramine acts quickly and can be useful in an emergency, but it causes drowsiness and may impair your ability to drive. If you need fast relief and are not operating machinery, it’s a reasonable choice while awaiting medical help.
How can I tell if my swelling is due to histamine or bradykinin?
Histamine reactions often come with itching, hives, or a known allergen exposure and respond to antihistamines. Bradykinin swelling usually lacks itch, may be linked to ACE‑inhibitor use or family history of hereditary angioedema, and does not improve with antihistamines.
Should I carry an epinephrine auto‑injector if I’ve never had a severe episode?
If you have a history of rapid facial swelling, throat tightness, or any episode that required emergency care, an auto‑injector is advisable. Discuss your case with a clinician to decide whether it’s necessary.





Tanna Dunlap
October 3, 2025 AT 01:47It’s frankly disgraceful how countless people gloss over the straightforward immunology and keep dialing emergency services without ever learning the difference between histamine and bradykinin.
Troy Freund
October 4, 2025 AT 19:27Whoa, this write‑up really shines a light on something most of us skim past. Knowing the mechanism lets you stay cool when the swelling hits and act fast.
Mauricio Banvard
October 6, 2025 AT 13:07What they don’t tell you is that the big pharma lobby deliberately buries the simple antihistamine protocols so we stay hooked on expensive biologics – a classic cover‑up.
Paul Hughes
October 8, 2025 AT 06:47Cool breakdown, really helpful. 👍 If you’ve ever wondered why the lips puff up so fast, now you’ve got the science behind it.
Mary Latham
October 10, 2025 AT 00:27i kno u think histamine is the only villain, but actually bradykinin can sneak in when you’re on ACE‑inhibitors – guess u missed that part.
Marie Green
October 11, 2025 AT 18:07Wow, thanks for the clear explanation. Very useful.
TOM PAUL
October 13, 2025 AT 11:47Take note, folks: keep a symptom diary, note every bite, pill, and sting. Spotting patterns early can save you a trip to the ER.
Ash Charles
October 15, 2025 AT 05:27Listen up – if you’re on an ACE inhibitor and get any swelling, STOP the drug immediately. Do it now, not later.
Michael GOUFIER
October 16, 2025 AT 23:07In reviewing the presented material, one must commend the thoroughness of the pathophysiological overview, yet it would benefit from a succinct summary table for rapid clinical reference.
michael Mc Laughlin
October 18, 2025 AT 16:47Great info, really helpful for people new to the topic keep it up
Luke Schoknceht
October 20, 2025 AT 10:27Honestly, the article tries to be balanced but ends up drowning in jargon. First, the distinction between H1 and H2 receptors is glossed over, leaving lay readers confused. Second, the table is a nice visual aid, yet it omits the crucial time‑frame for bradykinin‑mediated attacks, which can mislead someone into thinking antihistamines will always work. Third, the “quick comparison” section could have been expanded to include typical lab values for C1‑esterase deficiency. Finally, the emergency guidance is adequate, but it fails to stress the importance of calling EMS *before* administering epinephrine if airway compromise is imminent. All in all, a decent primer, but the devil’s in the details that were brushed aside.
mauricio gonzalez martinez
October 22, 2025 AT 04:07Got it.
Christian Freeman
October 23, 2025 AT 21:47The philosophical underpinning here is clear: we are at the mercy of tiny molecules, yet we wield powerful drugs to redirect them. Understanding that balance is what separates panic from preparedness.
julie shayla
October 25, 2025 AT 15:27Oh sure, because everyone just loves a good swelling episode-nothing says “fun weekend” like a suddenly puffy tongue. Maybe try not taking the meds that cause it, genius?
Super Mom
October 27, 2025 AT 08:07For parents dealing with kids who have recurrent angioedema, keep an epinephrine auto‑injector on hand, educate school staff, and track triggers in a simple notebook. Early intervention makes all the difference.
Jean Tredoux
October 29, 2025 AT 01:47They hide the real cause, sure, but the facts are simple: ACE inhibitors boost bradykinin, not histamine. No need for fancy jargon.
cedric Gicquiaud
October 30, 2025 AT 19:27Look, the mainstream narrative says antihistamines fix everything, but that’s a lie when you’re on an ACE inhibitor. Stop the drug, get a proper work‑up, and quit swallowing misinformation.
Mason Grandusky
November 1, 2025 AT 13:07Love the enthusiasm! If you’re experiencing repeated episodes, consider a prophylactic antihistamine regimen and schedule a follow‑up with an allergist to explore immunotherapy options.
Avinash Sinha
November 3, 2025 AT 06:47Let me unpack the drama of histamine‑driven angioedema in a way that even my most skeptical aunt can follow. First, imagine mast cells as tiny fireworks factories, bursting with histamine the moment an allergen flashes past. That histamine then darts to H1 and H2 receptors, opening the vascular gate like a busted dam-fluid rushes out, and you get that gloriously grotesque puffiness. Second, the timeline is spectacular: within seconds to a couple of minutes you’re staring at a swollen lip that looks like a cartoon character. Third, the itching and tingling are not just side effects; they’re the nervous system’s way of shouting “something’s wrong!” as the histamine also binds to sensory nerves. Fourth, the body’s response can be modulated with second‑generation antihistamines that calm the storm without making you feel like a zombie. Fifth, if you need an immediate fix, diphenhydramine steps in like a thunderclap, but it brings sleepiness as a bonus. Sixth, steroids act as the behind‑the‑scenes director, ensuring the swelling doesn’t make an encore appearance later.
Seventh, contrast this with bradykinin‑mediated angioedema, which sneaks in silently, often from ACE inhibitors, and refuses to respond to any antihistamine, leaving you helpless until you stop the offending drug or use a bradykinin antagonist. Eighth, that’s why doctors stress the importance of distinguishing the two; misdiagnosis leads to wasted meds and persistent danger. Ninth, you can tell them apart: histamine swelling comes with itch, rash, or hives, while bradykinin lacks those clues and often shows deeper tissue involvement. Tenth, a quick triage: ask yourself, “Did this happen after a known allergen? Is there itching?” If yes, you’re likely dealing with histamine. Eleventh, keep an epinephrine auto‑injector handy if airway swelling looms-time is of the essence.
Twelfth, for chronic sufferers, daily antihistamines can blunt the mast‑cell response, turning occasional flare‑ups into rare footnotes. Thirteenth, lifestyle tweaks-avoid known triggers, maintain a balanced gut microbiome, and manage stress-are proven to lower baseline mast‑cell reactivity. Fourteenth, never ignore a sudden tongue or throat swelling; even if you think it’s histamine, the airway can shut down in minutes. Fifteenth, always inform your healthcare team about any ACE inhibitors or similar meds you’re on; a simple drug swap can save your life. Sixteenth, when you finally get a proper diagnosis, celebrate the knowledge because now you hold the keys to prevent the next surprise. Finally, remember: knowledge is the antidote to panic, and this guide equips you with exactly that, turning a potentially terrifying episode into a manageable, even predictable, event.