How to Handle Breakthrough Bleeding While Taking Conjugated Estrogens USP

If you’re taking conjugated estrogens USP and suddenly notice spotting or heavier bleeding outside your expected cycle, you’re not alone. This is called breakthrough bleeding, and it’s one of the most common reasons people stop hormone therapy. It’s uncomfortable, confusing, and sometimes scary-but it’s rarely dangerous. Most of the time, it’s your body adjusting. But knowing when to worry and what to do next can make all the difference.
Why Breakthrough Bleeding Happens on Conjugated Estrogens USP
Conjugated estrogens USP is a form of estrogen used mainly for menopause symptoms like hot flashes and vaginal dryness. It’s often prescribed alone or with a progestin to protect the uterus. Breakthrough bleeding happens when the lining of the uterus (endometrium) grows unevenly because the hormone levels aren’t balanced just right.When you first start taking conjugated estrogens, your body is learning how to respond. The endometrium can become thicker than normal, and when it sheds in patches instead of all at once, you get spotting. This usually settles down after 3 to 6 months. But if you’ve been on it for over a year and bleeding starts again, something else might be going on.
Other triggers include missing a pill, taking it at different times each day, or interactions with other medications like antibiotics or seizure drugs. Even stress, major weight changes, or thyroid problems can throw off hormone balance enough to cause bleeding.
When to Call Your Doctor
Not all bleeding needs urgent care-but some signs mean it’s time to get checked. You should contact your healthcare provider if:- The bleeding is heavier than a normal period
- You’re passing clots larger than a quarter
- The bleeding lasts longer than 7 days
- You have bleeding after sex or after menopause has been confirmed (no periods for 12+ months)
- You feel dizzy, weak, or have severe abdominal pain
These could point to something more serious like uterine polyps, fibroids, endometrial hyperplasia, or even cancer. While these are rare, they’re easier to treat when caught early. Don’t wait to see if it "goes away on its own."
What Your Doctor Will Do
If you report breakthrough bleeding, your provider won’t just assume it’s normal. They’ll likely ask about your dosing history, other medications, and any recent changes in your life. Then they’ll probably order a few simple tests:- Transvaginal ultrasound to measure endometrial thickness
- Pap smear or endometrial biopsy if you’re over 35 or have risk factors
- Thyroid function and blood count tests to rule out anemia or hormonal imbalances
If everything looks normal, they might adjust your dose, switch you to a different formulation (like a patch or gel), or add a progestin if you’re not already taking one. Conjugated estrogens USP alone increases endometrial cancer risk over time, so most women with a uterus are prescribed a progestin alongside it.

What You Can Do at Home
While you wait to see your doctor or if they say it’s normal, here’s what helps:- Take your pill at the same time every day-even if you’re traveling. Set a phone reminder.
- Don’t skip doses. If you miss one, take it as soon as you remember. If it’s been more than 24 hours, skip it and go back to your regular schedule. Don’t double up.
- Track your bleeding in a journal or app. Note the date, flow (light, medium, heavy), color, and any pain. This helps your doctor spot patterns.
- Use pads instead of tampons during bleeding episodes. Tampons can make it harder to judge how much you’re losing and increase infection risk if you’re already on hormone therapy.
- Stay hydrated and eat iron-rich foods like spinach, lentils, red meat, or fortified cereals. Heavy bleeding can lead to low iron, which causes fatigue and dizziness.
Alternatives to Conjugated Estrogens USP
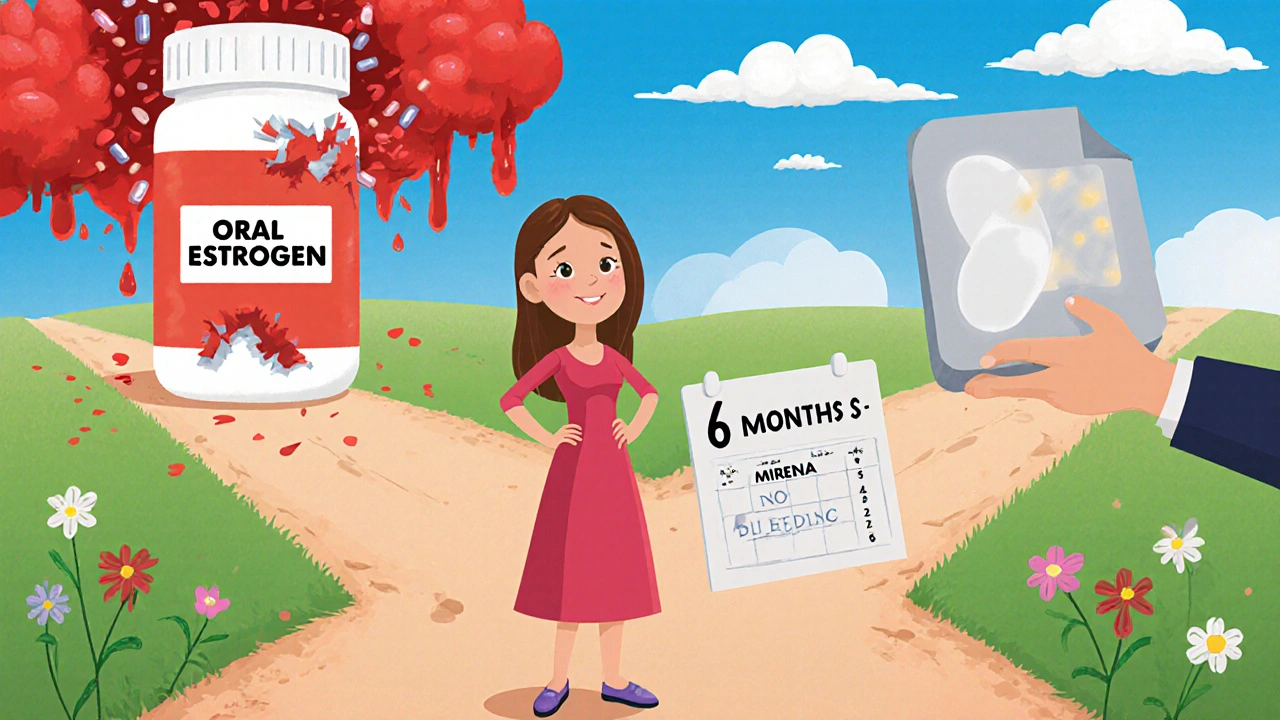
If breakthrough bleeding keeps happening and it’s affecting your quality of life, talk to your doctor about switching. There are other estrogen options that might be gentler on your system:- Estrogen patches (like Vivelle-Dot or Climara): Deliver steady hormone levels through the skin, avoiding the liver’s first-pass effect. Many women report less spotting.
- Estrogen gels (like Estrogel): Applied daily to the skin, they offer consistent absorption and fewer gastrointestinal side effects.
- Bioidentical estradiol: Structurally identical to the estrogen your body makes. Often prescribed in lower, more natural doses.
Some people also benefit from switching from oral conjugated estrogens to a low-dose intrauterine device (IUD) like Mirena, which releases progestin directly into the uterus. This can stop bleeding almost completely while still allowing systemic estrogen through a patch or pill.
How Long Does Breakthrough Bleeding Last?
For most people, spotting clears up within 3 to 6 months. But it’s not a race. Your body needs time to adapt. One study in the Journal of Clinical Endocrinology & Metabolism found that 60% of women on estrogen therapy had breakthrough bleeding in the first 3 months-but only 12% still had it after 12 months.If you’re past the 6-month mark and bleeding continues, it’s not normal. Don’t accept it as "just part of the process." Your doctor should reassess your treatment plan. There’s almost always a better option.
What Not to Do
Avoid these common mistakes:- Don’t stop your medication cold turkey. Stopping suddenly can cause withdrawal bleeding, worsen hot flashes, and even increase bone loss.
- Don’t use over-the-counter herbal supplements like black cohosh or red clover without talking to your doctor. They can interfere with estrogen metabolism.
- Don’t assume it’s "just aging." While hormone changes are normal, abnormal bleeding isn’t.
Bottom Line: Stay Calm, Stay Informed
Breakthrough bleeding on conjugated estrogens USP is common, but it’s not something you should ignore. Most cases are harmless and temporary. But it’s also your body’s way of signaling something’s off. Track it. Talk to your provider. Don’t settle for discomfort when better options exist.The goal isn’t just to stop the bleeding-it’s to find a treatment that works for your body without side effects. You deserve hormone therapy that supports your health, not disrupts it.
Is breakthrough bleeding normal on conjugated estrogens USP?
Yes, breakthrough bleeding is common in the first 3 to 6 months of starting conjugated estrogens USP, especially if you still have a uterus and aren’t taking a progestin. It usually improves as your body adjusts. But if it continues beyond 6 months, becomes heavy, or starts after you’ve been stable for a year, you should see your doctor.
Can I take ibuprofen for breakthrough bleeding?
Yes, over-the-counter ibuprofen can help reduce bleeding and cramping. It works by lowering prostaglandins, which cause uterine contractions. A typical dose is 200-400 mg every 6-8 hours during bleeding, but don’t use it long-term without checking with your doctor, especially if you have kidney issues or stomach ulcers.
Do I need a progestin with conjugated estrogens USP?
If you still have your uterus, yes-you almost always need a progestin. Estrogen alone thickens the uterine lining, which can lead to hyperplasia or cancer over time. Progestins like medroxyprogesterone or norethindrone help shed the lining safely. If you’ve had a hysterectomy, you don’t need it.
Can breakthrough bleeding mean I’m pregnant?
It’s very unlikely if you’re postmenopausal and on estrogen therapy, since ovulation stops. But if you’re under 45 and still having occasional periods, pregnancy is possible-even if you think you’re not fertile. A simple urine pregnancy test can rule it out in minutes.
Will switching to a patch reduce bleeding?
Many women find that switching from oral conjugated estrogens to a transdermal patch reduces breakthrough bleeding. Patches deliver estrogen steadily through the skin, avoiding the liver spikes that come with swallowing pills. This leads to more stable hormone levels and less uterine irritation.
How long should I wait before calling my doctor about bleeding?
If bleeding lasts more than 7 days, is heavy enough to soak through a pad every 2 hours, or happens after menopause (12+ months without periods), call your doctor right away. Don’t wait to see if it stops. Early evaluation can catch serious conditions before they become harder to treat.




Erica Lundy
November 18, 2025 AT 23:39Breakthrough bleeding, while clinically common, represents a profound disruption in the homeostatic equilibrium of endogenous hormonal signaling. The endometrial epithelium, under the influence of exogenous conjugated estrogens, undergoes aberrant proliferation without the counter-regulatory modulation of progestogenic agents-this is not merely a side effect, but a physiological misalignment requiring systematic recalibration.
One must consider the pharmacokinetic variance between oral administration and transdermal delivery: the first-pass hepatic metabolism induces pulsatile estrogen peaks, which destabilize estrogen receptor expression in the uterine mucosa. Patches, by contrast, sustain steady-state serum concentrations, thereby minimizing transcriptional noise in the endometrium.
It is ethically imperative that patients not be normalized into accepting chronic spotting as inevitable. Medicine ought to optimize, not accommodate, dysfunction. The persistence of bleeding beyond six months is not an adjustment-it is a failure of therapeutic design.
Moreover, the reliance on ibuprofen as a palliative masks the underlying pathophysiology. Prostaglandin suppression does not restore endometrial integrity; it merely dampens the symptom. A true therapeutic intervention must address the root: hormonal asymmetry.
And yet, the medical establishment often prioritizes convenience over precision. Why are bioidentical estradiol formulations not first-line? Why is the Mirena IUD, a marvel of localized progestogenic delivery, underutilized in conjunction with systemic estrogen?
We must move beyond the paradigm of ‘tolerating side effects’ and toward the principle of individualized hormonal architecture. The body does not adapt to imbalance-it resists it. Bleeding is its protest.
Patients deserve therapies that honor biological fidelity, not pharmaceutical compromises.
- Erica Lundy, Ph.D. (Philosophy of Medicine)
Kevin Jones
November 20, 2025 AT 23:17Oral CEE → hepatic first-pass → supraphysiologic estrogen spikes → endometrial chaos.
Transdermal = steady-state = no drama.
Progestin non-negotiable if uterus intact.
Stop taking pills at 3 a.m. and wonder why you’re bleeding.
Case closed.
Premanka Goswami
November 22, 2025 AT 07:07Let me tell you something they don’t want you to know.
Conjugated estrogens USP? It’s not just hormones-it’s a corporate ploy to keep women dependent. Big Pharma knows if you bleed, you’ll keep coming back. They don’t care about your uterine lining-they care about your monthly prescription refill.
And why do they push patches? Because they cost 3x more. Same active ingredient. Same effect. But now you’re paying for ‘premium delivery.’
They’ll tell you to track your bleeding in an app. Meanwhile, your insurance won’t cover bioidentical estradiol because it’s not patentable.
And the ‘progestin’ they add? Medroxyprogesterone? That’s synthetic progesterone. It’s not even real progesterone. It’s a steroid impostor. That’s why you still bleed.
Real solution? Stop taking everything. Go natural. Eat flaxseed. Exercise. Sleep. Your body didn’t need this in the first place.
They call it ‘menopause.’ I call it a manufactured crisis.
Wake up.
- Premanka Goswami, Independent Researcher
Alexis Paredes Gallego
November 24, 2025 AT 01:22Okay but what if the bleeding isn’t from the estrogen at all?
What if it’s the glyphosate in your soy milk? Or the endocrine disruptors in your shampoo? Or the fact that your doctor prescribed this without checking your thyroid? Or worse-what if you’re being gaslit into thinking this is normal?
I’ve seen women bleed for 18 months and get told ‘it’s just adjustment.’
Then they get diagnosed with stage 2 endometrial cancer.
They don’t tell you this, but estrogen therapy is a gamble. And the casino is your uterus.
And don’t even get me started on how they use ‘IUD’ as a buzzword to sell you a $1000 device while you’re on a $20 pill.
They’re not helping you.
They’re profiting from your confusion.
- Alexis Paredes Gallego, Survivor of the Hormone Industrial Complex
Saket Sharma
November 24, 2025 AT 13:24CEC: Conjugated Equine Estrogens. Not human. Not bioidentical.
Oral bioavailability: 50%? 30%? Who knows. Liver metabolizes it into 17-alpha-estradiol, 16-alpha-hydroxyestrone-messy metabolites.
Progestin? Medroxyprogesterone acetate? That’s a synthetic progestin. Not progesterone. Causes mood swings, weight gain, and yes-breakthrough bleeding.
Switch to transdermal estradiol + micronized progesterone.
Done.
Stop taking the horse pee.
- Saket Sharma, MD (Endocrinology)
Shravan Jain
November 26, 2025 AT 05:35yea so i read the whole thing and i think its kinda bs.
they say 'take it at same time' like its that hard? i take mine at 10pm, sometimes 1am, sometimes i forget. still got bleeding. so what.
and 'track in app'? why? i just use a notebook. and i write 'spotting' or 'heavy' or 'fucking hell'.
and ibuprofen? yeah it works. i take 400mg and its gone. why overcomplicate?
also, 'bioidentical'? sounds like a trend. i bet its just more expensive.
and why do they say 'don't stop cold turkey'? like i'm gonna just quit? i'm not a junkie.
just take the pill. if it bleeds, wait. if it keeps bleeding, go to doc. simple.
why do people make everything so dramatic?
- shravan jain, not a doctor but i read the internet
mithun mohanta
November 26, 2025 AT 17:52Let me just say-this entire discourse is a symptom of our medical industrial complex’s pathological obsession with control.
They want you to track bleeding. To log apps. To set phone reminders. To swallow pills at 8:03 AM precisely. As if your body is a poorly calibrated machine.
But here’s the truth: your body is not a machine. It is a living, breathing, evolving ecosystem. And when you force it to accept equine-derived estrogen-yes, horse urine, folks-it responds with protest.
Why is transdermal delivery ‘better’? Because it bypasses the liver’s metabolic tyranny. But no one talks about the fact that the liver evolved for a reason.
And progestins? They’re not ‘progestins’-they’re synthetic imposters. Real progesterone is a neurosteroid. It calms your nervous system. Medroxyprogesterone? It makes you depressed.
So yes-switch to estradiol patches.
Yes-use micronized progesterone.
Yes-ditch the horse pee.
But more importantly: stop believing that your body needs fixing.
It’s not broken. It’s just being lied to.
- mithun mohanta, Rebellious Humanist
deepak kumar
November 28, 2025 AT 04:15Hey everyone, I've been on this for 2 years now and I want to share what actually worked for me.
Started with CEE oral-spotting every week. Felt awful.
Switched to estradiol patch (Vivelle-Dot 0.1 mg) + micronized progesterone 100 mg at night. No more bleeding after 6 weeks.
Also switched to taking progesterone only for 12 days/month-not daily. That made a huge difference in mood and energy.
And yes-I stopped taking ibuprofen daily. Only used it for cramps. Didn’t need it for bleeding control.
Also, I started eating more lentils, spinach, and pumpkin seeds. Iron levels went up, fatigue disappeared.
Don’t panic. Don’t stop cold turkey. But don’t settle either.
Your doctor should be your partner-not your boss.
Find one who listens. Try the patch + micronized progesterone. It’s not magic. But it’s science that actually works.
And no-it’s not about horse pee. It’s about matching your body’s rhythm.
You got this.
- Deepak Kumar, Menopause Warrior