When Your Doctor Might Prescribe Brand-Name Only and Why
Most prescriptions you get filled are generics. They work just as well, cost a fraction of the price, and are approved by the FDA. So why would your doctor ever write a prescription for the brand-name version? It’s not about preference. It’s not about profit. In most cases, it’s not even about the doctor being out of touch. Sometimes, it’s the only safe choice.
When Generic Isn’t Good Enough
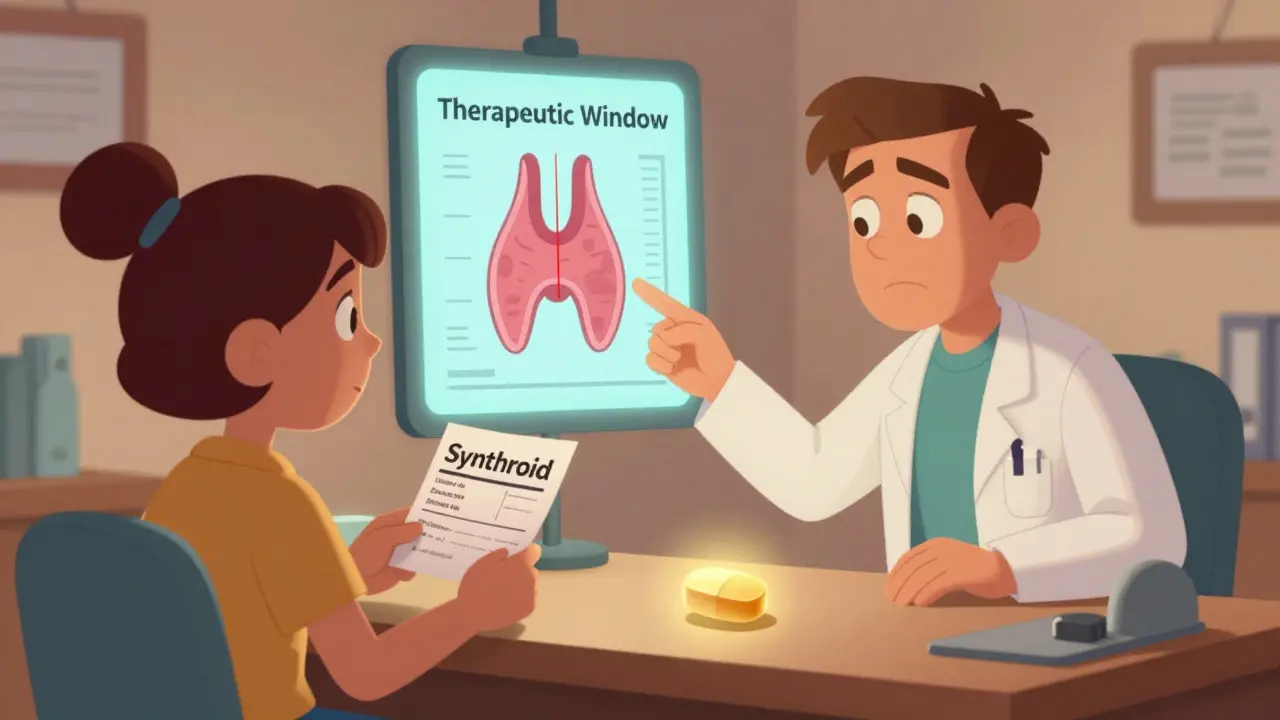
For the vast majority of medications-antibiotics, blood pressure pills, cholesterol drugs, even antidepressants-generics are identical in effect. The FDA requires them to deliver the same active ingredient, in the same amount, at the same rate as the brand. That’s the rule. And it works. Studies involving over 100,000 patients show no difference in outcomes between brand and generic statins, ACE inhibitors, or metformin. But there’s a small group of drugs where even tiny differences matter. These are called narrow therapeutic index (NTI) drugs. With these, the gap between a dose that works and one that’s dangerous is razor-thin. A 5% change in blood levels can mean the difference between controlling your seizures or having one. Or between keeping your thyroid in balance or slipping into fatigue, depression, or heart trouble. That’s why doctors often insist on brand-name versions for drugs like:- Levothyroxine (Synthroid) for hypothyroidism
- Warfarin (Coumadin) for blood thinning
- Levetiracetam (Keppra) for epilepsy
- Cyclosporine (Neoral) for organ transplants
What Happens When You Switch Generics?
A 2019 study tracked 1,200 people with epilepsy who were switched from brand-name Keppra to a generic version. Twelve point seven percent had breakthrough seizures. Only 4.3% of those who stayed on the brand did. That’s a nearly threefold increase. That’s not a coincidence. That’s biology. Patients on levothyroxine report similar stories. On Reddit’s pharmacy forums, hundreds describe mood swings, weight gain, and severe fatigue after switching to a generic. One woman wrote: “I switched from Synthroid to generic twice. Both times, I developed depression so bad I couldn’t get out of bed. Switched back-within two weeks, I was myself again.” It’s not that generics are unsafe. It’s that their consistency isn’t guaranteed across manufacturers. One batch of generic levothyroxine might come from Company A, the next from Company B. Their inactive ingredients-dyes, binders, fillers-can differ. For most people, that’s invisible. For someone with a sensitive thyroid or nervous system, it’s enough to throw everything off.Why Doctors Still Prescribe Brand When They Don’t Have To
Here’s the uncomfortable truth: a lot of brand-name prescriptions aren’t medically necessary. A 2020 study in Health Affairs found only 3% of brand-only prescriptions had real clinical justification. The rest? Patient requests. Doctor habits. Marketing. Doctors hear “My cousin took the brand and it worked better.” They see ads for the latest version of a drug. They’re trained to say “Lipitor” instead of “atorvastatin.” Research shows that when a doctor says the brand name, they’re more likely to prescribe it-even if they know the generic is equivalent. Pharmaceutical reps visit doctors’ offices. They hand out samples. They talk about “reliability” and “consistency.” They don’t mention the $400 price tag. And patients? They’ve been told for years that brand = better. That’s not always true. But it’s hard to unlearn.
What You Can Do
If your doctor writes a brand-only prescription, ask: Why? Not in a confrontational way. Just say: “I know generics are cheaper. Is there a medical reason you’re asking for the brand?” If it’s an NTI drug-thyroid, seizure, blood thinner-then yes, stick with the brand. But if it’s for something like lisinopril, metformin, or omeprazole? Ask if the generic is an option. Most of the time, it is. And if your pharmacist tries to swap your brand for a generic without permission? That’s legal in 49 states-unless your doctor wrote “dispense as written” or “brand medically necessary.” If you’re on an NTI drug and that note isn’t there, speak up. Your life could depend on it.Insurance and Costs: The Hidden Battle
Brand-name drugs cost 80 to 85% more than generics. On average, a brand prescription runs $471. A generic? Around $14. That’s not a typo. When your doctor prescribes a brand without a clear medical reason, your insurance may deny coverage. You’ll be stuck paying full price. A 2021 Kaiser Family Foundation survey found 42% of patients paid hundreds more each year because their doctor prescribed a brand unnecessarily. If your doctor insists on the brand, they’ll need to write “medical necessity” on the prescription. Your insurer will then require prior authorization. That means paperwork. A 72-hour wait. And no guarantee they’ll approve it. For NTI drugs, approval rates are high-up to 89%. For proton pump inhibitors? Only 45%. So if your doctor wants to prescribe omeprazole instead of generic esomeprazole for heartburn, don’t be surprised if your insurance says no.
What’s Changing?
The FDA is paying more attention. In 2023, they started requiring generic manufacturers to make their pills look like the brand-same shape, same color, same markings. Why? Because patients confuse different generics. One pill looks like another. That leads to errors. There’s also a new option: authorized generics. These are made by the original brand company but sold under a generic label. Same formula, same factory, same quality control. No variability between batches. They’re cheaper than the brand but more consistent than other generics. Ask your pharmacist if one exists for your drug. And slowly, prescribers are learning. Electronic health records now flag when a generic is available. Some systems even suggest alternatives. But studies show these alerts only reduce inappropriate prescribing by about 19%. Real change needs education-and patient advocacy.Bottom Line
Generics are safe, effective, and save billions every year. For 90% of prescriptions, they’re the smart choice. But for a few critical drugs-thyroid, epilepsy, blood thinners-the differences matter. Don’t assume your doctor knows. Don’t assume your pharmacist will protect you. Ask questions. Know your drug. Know your options. If your doctor says “brand only,” make sure it’s because it’s medically necessary-not because it’s easier, more familiar, or more profitable. Your health isn’t a marketing campaign. It’s your body. And you deserve to know why you’re paying what you’re paying.Can I ask my doctor to switch from brand-name to generic?
Yes, absolutely. You have the right to ask why a brand-name drug was prescribed and whether a generic is an option. For most medications, the answer will be yes. For narrow therapeutic index drugs like levothyroxine or levetiracetam, the doctor may say no-but they should explain why. Always ask for the reasoning, not just accept it.
Why do some pharmacies refuse to substitute generics even when the doctor didn’t say "do not substitute"?
In 49 U.S. states and D.C., pharmacists are allowed to substitute generics unless the doctor specifically says "dispense as written" or "brand medically necessary." But some pharmacies have internal policies to avoid liability, especially with NTI drugs. They may call the doctor to confirm, even if the law doesn’t require it. It’s a safety precaution, not a refusal.
Are generic drugs less effective than brand-name drugs?
For most drugs, no. The FDA requires generics to be bioequivalent-meaning they deliver the same active ingredient at the same rate and strength. Large studies involving tens of thousands of patients confirm this. But for drugs with a narrow therapeutic index, small differences in how the drug is absorbed can matter. That’s why consistency matters more than cost for those specific medications.
What does "dispense as written" mean on a prescription?
It means the prescriber is asking the pharmacist to give exactly the drug they wrote-no substitutions. This overrides state laws that allow generic substitution. It’s legally binding. If the doctor doesn’t write this, the pharmacist can usually swap in a generic unless it’s an NTI drug and the pharmacy has its own policy to avoid risk.
Can I get the brand-name drug if my insurance denies it?
You can pay out of pocket, but it will cost significantly more-sometimes hundreds of dollars more per month. Before doing that, ask your doctor to submit a prior authorization request with medical justification. If you’re on an NTI drug, approval is likely. If not, you may be paying extra for no clinical benefit.
Are authorized generics the same as the brand-name drug?
Yes. Authorized generics are made by the original brand manufacturer but sold under a generic label. They have the same active ingredient, inactive ingredients, and manufacturing process as the brand. The only difference is the packaging and price. They’re a good middle ground if you need consistency but can’t afford the brand.
Why do some people have side effects from generics but not the brand?
It’s usually due to inactive ingredients-fillers, dyes, preservatives-that vary between manufacturers. For most people, these don’t matter. But if you’re sensitive to certain dyes (like FD&C red) or have a rare intolerance to a binder, you might react to one generic but not another-or to the brand. If you notice new side effects after switching, report them to your doctor and pharmacist.





jeremy carroll
December 15, 2025 AT 13:00bro i switched my thyroid med to generic and felt like a zombie for 3 weeks. just wanted to cry and sleep forever. went back to synthroid and boom, human again. not even joking. my dog noticed the difference.
Thomas Anderson
December 15, 2025 AT 23:29my pharmacist asked if i wanted the generic for my blood thinner and i said no. he looked at me like i was crazy. i told him i read the study about seizures. he just nodded and said, 'smart move.'
Dwayne hiers
December 16, 2025 AT 14:24the bioequivalence standards for NTI drugs are inherently flawed because they rely on population-level AUC and Cmax thresholds, which mask inter-individual variability in absorption kinetics. even if a generic meets FDA’s 80–125% confidence interval, the pharmacokinetic profile may still induce subtherapeutic or toxic troughs in susceptible individuals due to altered dissolution rates from excipient differences. this is why therapeutic drug monitoring is critical when switching - and why some clinicians err on the side of brand consistency.
Jonny Moran
December 17, 2025 AT 06:16if you’re on levothyroxine and you feel off after a switch, don’t brush it off as ‘just stress.’ your thyroid doesn’t care about your budget. ask for the brand. if your doc pushes back, ask for a copy of the study that says it’s fine. most won’t have one. and if they do? great. but don’t let cost override your biology.
Natalie Koeber
December 17, 2025 AT 11:34you think this is about medicine? nah. big pharma owns the FDA, the doctors, the pharmacies. they want you on the brand so they can charge $500 a month. the ‘narrow therapeutic index’ thing? a distraction. they’ve been doing this since the 80s. even the ‘authorized generics’? still made by the same corporations. wake up.
Rulich Pretorius
December 18, 2025 AT 04:13the real issue isn’t whether generics work - it’s whether our system allows patients to make informed choices without being financially punished. we’ve turned healthcare into a transaction, not a relationship. if you’re on warfarin or levetiracetam, you’re not just taking a pill - you’re navigating a minefield of corporate incentives, insurance bureaucracy, and inconsistent manufacturing. your body deserves better than a cost-cutting algorithm.
ask your doctor for the reason. write it down. if they can’t give you a clear, evidence-based answer - then question it. not out of fear, but out of respect for your own health.
Daniel Thompson
December 19, 2025 AT 08:46As a physician who has prescribed both brand and generic medications for over two decades, I can attest that the clinical distinction for NTI drugs is empirically valid. However, the systemic failure lies in the lack of standardized labeling across generic manufacturers, which leads to confusion among both clinicians and patients. Furthermore, the absence of mandatory post-market pharmacovigilance for generic formulations exacerbates underreporting of adverse events. I now routinely document ‘dispense as written’ for levothyroxine, warfarin, and antiepileptics - not out of habit, but out of liability awareness and clinical responsibility.
Wade Mercer
December 20, 2025 AT 07:46people who complain about generics are just lazy. if you can’t handle a $14 pill instead of $470, maybe you shouldn’t be on medication at all. this country is full of entitled whiners who think their body is special. generics save lives by making treatment accessible. stop being dramatic.