Drug Safety: Understanding Risks, Interactions, and How to Stay Protected
When you take a medication, drug safety, the practice of using medicines in a way that minimizes harm while maximizing benefit. Also known as medication safety, it’s not just about following the label—it’s about knowing what else in your life might turn that pill into a problem. Every year, hundreds of thousands of people end up in emergency rooms because of preventable drug mistakes. Some mix pills with tea. Others skip doses because the label was unclear. A few don’t realize their blood thinner is working differently because their kidneys changed. Drug safety isn’t a one-time check—it’s a daily habit.
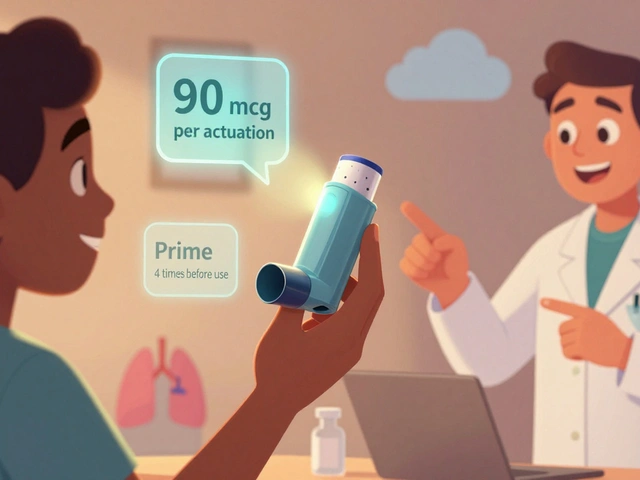
It starts with understanding adverse drug reactions, unintended and harmful responses to medications at normal doses. These aren’t always obvious. A headache from metformin? Maybe just your stomach adjusting. But if your skin turns yellow and your urine darkens, that’s lactic acidosis—rare, but deadly. Then there’s drug interactions, when one medicine changes how another works in your body. Zinc and antibiotics? Take them together and you might as well be swallowing sugar. Dairy and tetracycline? One glass of milk can slash absorption by over 90%. Even herbal teas like chamomile or green tea can mess with birth control or blood thinners. These aren’t myths—they’re documented, measurable risks.
And then there’s the system itself. controlled substances, drugs with high potential for abuse, classified by the DEA into five schedules, come with labels that tell you how many refills you get, who can prescribe them, and what legal penalties apply if you share them. A Schedule II opioid like oxycodone isn’t just stronger—it’s tightly locked down. A Schedule IV benzodiazepine like Xanax? Still risky, but refill rules are looser. Knowing the difference isn’t legal trivia—it’s your protection. Pharmacists can’t swap combination pills just because they’re cheaper. Generic drugs aren’t always interchangeable. And if you’re on a blood thinner like apixaban or rivaroxaban, your kidney function isn’t just a number—it’s the reason your dose changed last month.
Drug safety isn’t about fear. It’s about awareness. It’s reading the DailyMed label to check for new warnings. It’s using FAERS reports to see what others experienced. It’s asking if your IVIG therapy is the right fit for your autoimmune condition, or if your naloxone kit is even in the same room as your opioids. It’s knowing that breakthrough bleeding on estrogen isn’t always normal, and that keratosis pilaris cream won’t help your COPD. The posts below cover exactly these moments—the real-life decisions that keep you safe. No fluff. No guesswork. Just what you need to know before the next pill, patch, or injection.

Medical Alert Bracelets: When and Why They Matter for Drug Safety
Medical alert bracelets save lives by giving first responders instant access to critical drug info during emergencies. Learn who needs one, what to engrave, and how to avoid the most common mistakes that make them useless.
Categories
- Medications (71)
- Health and Medicine (62)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)