Variceal Bleeding: How Banding, Beta-Blockers, and Prevention Save Lives
When your liver is damaged by cirrhosis, pressure builds up in the veins that carry blood to it. This pressure forces blood to find new paths-through fragile, swollen veins in your esophagus or stomach. These are called varices. And when they burst, it’s not just a medical emergency-it’s a fight for your life. About 1 in 5 people who bleed from varices die within six weeks. But here’s the good news: we know exactly how to stop it, prevent it from coming back, and save lives. The tools are simple, proven, and available: banding, beta-blockers, and smart prevention.
What Causes Variceal Bleeding?
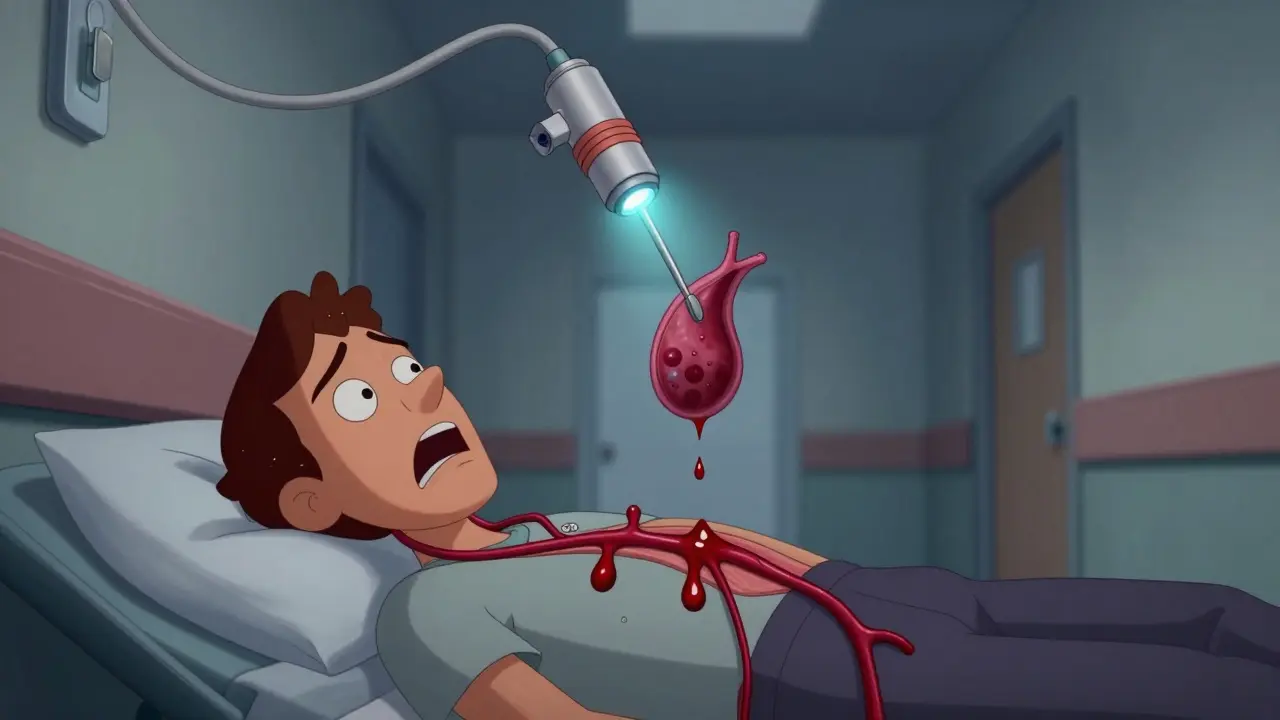
Variceal bleeding doesn’t happen out of nowhere. It’s the end result of years of liver damage, usually from alcohol, hepatitis, or fatty liver disease. When the liver scars (cirrhosis), it blocks blood flow. The pressure in the portal vein-your liver’s main blood supply-rises above 10 mmHg. Once it hits 12 mmHg or higher, veins in your esophagus or stomach swell like overfilled balloons. They’re thin-walled, fragile, and under massive strain. A cough, a bowel movement, or even nothing at all can make them rupture.That’s when you start vomiting blood, passing black, tarry stools, or feel dizzy and weak. It’s sudden. It’s scary. And it demands immediate action. Delaying treatment by even a few hours can mean the difference between survival and death.
Endoscopic Band Ligation: The Gold Standard for Stopping Bleeding
If you’re bleeding from varices, the first thing doctors do is get you to an endoscopy suite-fast. The clock starts ticking the moment you walk in. Guidelines say you need banding within 12 hours. That’s not a suggestion. It’s life-or-death timing.Endoscopic band ligation (EBL) is a procedure where a doctor uses a thin scope with a tiny device on the end to place rubber bands around the swollen veins. The bands cut off blood flow. The varices shrink, scar, and disappear over time. It’s not surgery. It’s minimally invasive. And it works.
Studies show that banding stops active bleeding in 90 to 95% of cases. That’s far better than older methods like injecting chemicals (sclerotherapy), which caused more complications like strictures and infections. Modern multi-band devices, like the Boston Scientific Six-Shot, can treat multiple varices in one pass, cutting procedure time by 35%. Most patients need 3 to 4 sessions, spaced 1 to 2 weeks apart, to fully clear the varices.
But it’s not perfect. If you’re bleeding heavily, the blood can obscure the view, making banding harder. In those cases, success drops to 85% or lower. And afterward, many patients report throat pain for weeks. Swallowing feels like swallowing glass. It’s uncomfortable-but it’s better than dying.
Beta-Blockers: The Silent Guardians Against Rebleeding
Stopping the bleeding is only half the battle. The real threat is it coming back. Without treatment, more than half of patients bleed again within a year. That’s where beta-blockers come in.Non-selective beta-blockers like propranolol and carvedilol don’t just lower your heart rate-they lower pressure in your liver’s blood vessels. They reduce cardiac output and shrink blood flow to the gut. The goal? Lower your hepatic venous pressure gradient (HVPG) to under 12 mmHg-or by at least 20% from baseline. That’s the sweet spot where bleeding risk drops dramatically.
Carvedilol is now preferred over propranolol. It’s more effective at lowering portal pressure-22% versus 15%. And it cuts rebleeding risk by about half. Propranolol costs $4 to $10 a month. Carvedilol? Around $25 to $40. But if you can tolerate it, carvedilol gives you better protection.
Here’s the catch: not everyone can take them. If you have asthma, a slow heart rate, or heart failure, beta-blockers can be dangerous. Side effects like fatigue, dizziness, and low blood pressure force 25 to 30% of patients to stop taking them. One patient on Reddit said, “Propranolol made me so tired I couldn’t get out of bed.” Another switched to carvedilol and said, “It worked better-but costs $35 a month.”
That’s why doctors don’t use beta-blockers alone during active bleeding. They’re for prevention. During an emergency, you get banding plus a short-term IV drug like terlipressin or octreotide. Beta-blockers are your long-term shield.

When Banding Isn’t Enough: Other Options
Not all varices are the same. If you have bleeding from the stomach (gastric varices), banding isn’t as effective. In those cases, doctors may use balloon-occluded retrograde transvenous obliteration (BRTO). It’s a catheter-based procedure that plugs off the vein from the inside and injects a glue-like substance. Studies show it cuts 30-day mortality nearly in half compared to banding alone.For the highest-risk patients-those with Child-Pugh B or C cirrhosis and active bleeding-TIPS (transjugular intrahepatic portosystemic shunt) is the most powerful tool. It creates a tunnel inside the liver to redirect blood flow and slash pressure. One-year survival jumps from 61% with standard care to 86% with TIPS. But there’s a trade-off: up to 30% of patients develop hepatic encephalopathy-confusion, memory loss, even coma-because toxins bypass the liver.
And here’s the reality check: only 45% of U.S. hospitals have interventional radiologists who can do TIPS within 24 hours. That means for many, it’s not an option-unless you’re at a major center.
Prevention: The Most Important Step
The best way to avoid variceal bleeding is to never let it happen in the first place. If you have cirrhosis but haven’t bled yet, you’re in the primary prevention phase. For that, guidelines now recommend carvedilol for high-risk patients-those with medium or large varices. Studies show it’s just as good as banding at preventing the first bleed.But prevention isn’t just medication. It’s avoiding alcohol completely. It’s getting vaccinated for hepatitis A and B. It’s managing your weight and blood sugar. It’s regular endoscopies every 1 to 2 years to check for varices. And it’s knowing the signs: vomiting blood, dark stools, sudden weakness. If you have cirrhosis and feel any of these, go to the ER. Don’t wait.
Even with perfect care, 65% of patients still have at least one rebleeding episode within a year. That’s why ongoing monitoring is non-negotiable. Your care team-gastroenterologist, liver specialist, nurse navigator-needs to be in constant contact with you. The American Liver Foundation’s nurse navigator program helps 12,000 patients a year coordinate care, manage meds, and find support. You don’t have to do this alone.

The Bigger Picture: Cost, Access, and Future Hope
In the U.S., about 250,000 people bleed from varices each year. The cost? $2.8 billion. Banding runs $1,200 to $1,800 per session. Beta-blockers are cheap. But access isn’t equal. Uninsured patients die at a rate 35% higher than those with insurance. Rural hospitals often lack endoscopy teams. Delays happen. Only 68% of patients get endoscopy within the critical 12-hour window.But hope is growing. In 2023, the FDA approved a long-acting form of octreotide that only needs monthly shots instead of daily infusions. That could improve adherence. In 2024, new guidelines may recommend carvedilol as first-line for primary prevention-bypassing banding altogether for some patients. And research is underway for AI tools that predict who’s most likely to bleed before it happens.
One expert put it best: “Integration of artificial intelligence for early bleeding prediction combined with novel pharmacotherapies could reduce variceal bleeding mortality by 40% within the next decade.” That’s not science fiction. It’s the next frontier.
What You Need to Do Right Now
If you or someone you love has cirrhosis:- Ask your doctor if you have varices-and how big they are.
- If you haven’t bled but have medium or large varices, ask about carvedilol.
- If you’ve bled before, you need banding plus beta-blockers. No exceptions.
- Know the warning signs of bleeding. Act immediately.
- Never drink alcohol. Ever.
- Get your hepatitis vaccines if you haven’t.
- Find a liver specialist and stick with them.
This isn’t a condition you manage on your own. It takes a team. But with the right tools-banding, beta-blockers, and relentless prevention-you can outlive your diagnosis.
Can variceal bleeding be prevented without banding?
Yes, for people who haven’t bled yet, non-selective beta-blockers like carvedilol can prevent the first bleed in many cases. For high-risk patients with medium or large varices, carvedilol is now recommended as a first-line option. But once bleeding happens, banding becomes essential to stop the immediate bleed and reduce rebleeding risk.
How long does it take for beta-blockers to work?
Beta-blockers start lowering portal pressure within days, but it takes weeks to reach the full effect. Doctors usually start with a low dose and slowly increase it over several weeks while monitoring heart rate and blood pressure. The goal is to reach the highest tolerated dose that lowers your hepatic venous pressure gradient by at least 20% or below 12 mmHg.
Is endoscopic banding painful?
The procedure itself is done under sedation, so you won’t feel it. Afterward, many patients report sore throat, difficulty swallowing, or chest discomfort for 1 to 2 weeks. It feels like a bad sore throat or even heartburn. These symptoms usually improve on their own. Pain medications and soft foods help. Severe or lasting pain should be reported to your doctor.
Can I stop taking beta-blockers if I feel fine?
No. Beta-blockers are not a cure-they’re a lifelong shield. Stopping them-even if you feel fine-can cause portal pressure to spike again, putting you at high risk for rebleeding. Most patients need to take them indefinitely. If side effects are too strong, talk to your doctor about switching to a different beta-blocker or adjusting the dose. Never stop on your own.
What happens if I miss a banding session?
Missing a session increases your risk of rebleeding. Varices don’t disappear on their own. Each session removes more of them, but they can regrow if treatment is interrupted. If you can’t make an appointment, call your clinic immediately. Many centers have emergency slots for patients who fall behind. Delaying treatment could mean another hospital stay-or worse.
Are there new treatments on the horizon?
Yes. A new long-acting octreotide (monthly injection) improves adherence. The PORTAS trial is testing a simpler, more widely available version of TIPS that could be done in more hospitals. AI tools are being developed to predict bleeding risk before it happens. And research into new drugs that directly reduce portal pressure without slowing the heart is underway. These won’t replace banding or beta-blockers soon, but they’ll add powerful new tools to the toolbox.
Next Steps: What to Do After Diagnosis
If you’ve been diagnosed with cirrhosis or varices:- Get a liver specialist (hepatologist) on your team.
- Ask for an endoscopy to check for varices.
- If you have varices, ask whether you need beta-blockers or banding.
- Set up reminders for medications and follow-up appointments.
- Join a patient support group-many find strength in shared experience.
- Keep your alcohol intake at zero.
- Know your emergency signs and act fast.
Variceal bleeding is serious-but it’s not inevitable. With the right care, you can live years, even decades, after diagnosis. The tools are here. The knowledge is proven. What matters now is acting on it.






Aayush Khandelwal
December 29, 2025 AT 13:31Man, this post is a masterclass in portal hypertension management. Banding’s the MVP, no doubt - but the real unsung hero is carvedilol’s dual alpha/beta blockade. That 22% HVPG reduction isn’t just stats, it’s a literal lifeline. And let’s not forget the multi-band devices - Boston Scientific’s Six-Shot cuts procedural time like a chainsaw through butter. We’re talking about reducing ICU stays, not just bleeding episodes. This isn’t medicine, it’s precision engineering of the circulatory system.
Hayley Ash
December 30, 2025 AT 01:14Henry Ward
December 31, 2025 AT 07:50People still think beta-blockers are ‘safe’? Tell that to the guy who crashed his truck because propranolol turned him into a zombie. And don’t get me started on ‘carvedilol is better’ - it’s just a more expensive way to make people feel like garbage. Meanwhile, hospitals are skipping endoscopy because they’re understaffed. This whole system is a scam. You think a $4 pill is going to fix cirrhosis caused by 20 years of binge drinking? Wake up. It’s not medicine - it’s damage control for people who refuse to change.
henry mateo
December 31, 2025 AT 20:08just read this whole thing and wow. i had no idea banding was so effective. i think i might have a friend who’s got cirrhosis and he’s been skipping his meds because he says ‘he feels fine’ - i’m gonna send him this. also i think i spelled ‘beta-blockers’ wrong in my text to him lol. sorry. but seriously thank you for writing this. it’s so clear.
Kunal Karakoti
January 2, 2026 AT 19:57It’s fascinating how medicine has evolved from brute-force interventions to nuanced modulation of hemodynamics. Banding is reactive, beta-blockers are prophylactic, and TIPS is a bypass - but all three are essentially attempts to reroute suffering. The real question isn’t which tool works best, but whether we’re treating the disease or merely the symptom. If the liver is a broken pump, are we fixing the pump… or just building better hoses around it?
Kelly Gerrard
January 3, 2026 AT 15:11Every single person reading this needs to understand one thing: cirrhosis is not a sentence. It is a challenge. And you have the power to meet it with discipline. No alcohol. No excuses. Take your meds. Show up for your endoscopies. Your life is not a suggestion. It is a responsibility. And if you don’t take it seriously - you are not just hurting yourself. You are wasting the work of every doctor, nurse, and researcher who fought to give you this chance.
Glendon Cone
January 4, 2026 AT 01:49Man this is wild. I had no idea carvedilol was that much better than propranolol 😮. And that long-acting octreotide thing? That’s like the medical version of a monthly subscription box for survival. 🙌 Also, I’m gonna start reminding my uncle to get his endoscopy. He’s been putting it off for 2 years. Time to be the annoying friend who texts ‘did u go yet?’ every week. 😅
Sandeep Mishra
January 5, 2026 AT 11:56For anyone in India reading this - yes, these treatments exist here. Not everywhere, but in major centers like AIIMS, PGIMER, or Apollo. Banding costs maybe 15k INR per session. Carvedilol? Around 300 rupees a month. You don’t need to go to the US to get life-saving care. What you need is to ask. To insist. To not accept ‘we don’t have it’ as an answer. Your liver doesn’t care about your bank account. It only cares if you show up.
Joseph Corry
January 5, 2026 AT 15:28How quaint. We have a ‘gold standard’ because we’ve stopped asking deeper questions. Banding treats the varix, but not the fibrosis. Beta-blockers reduce pressure, but don’t reverse endothelial dysfunction. TIPS creates a shunt, but accelerates encephalopathy. We’re playing whack-a-mole with physiology. The real innovation won’t come from a rubber band or a pill - it’ll come when we stop seeing the liver as a broken pipe and start seeing it as a collapsed ecosystem. Until then, we’re just rearranging deck chairs on the Titanic.
Colin L
January 6, 2026 AT 04:23Let me tell you about my cousin who got variceal bleeding. He was 47, worked in logistics, drank a six-pack every night for 15 years, never saw a doctor until he vomited blood into a bucket at 3am. They did banding, he got carvedilol, he was fine for 11 months - then he had a beer ‘just one’ because his buddy was celebrating his promotion. He bled again. They tried TIPS but his liver was too far gone. He died in the ICU after 17 days. They didn’t even have a proper endoscopy unit at his local hospital. They had to transfer him 120 miles. He was in shock before they even got him on the ambulance. So yeah, this post is great. But here’s the truth: medicine is useless if the patient doesn’t care. And most of them don’t. They wait until they’re dying. And then they blame the system. But the system didn’t make him drink. He did. And now he’s dead. And I’m tired of pretending this is about pills and procedures. It’s about will. And most people don’t have it.