Deep Vein Thrombosis (DVT): What You Need to Know Now
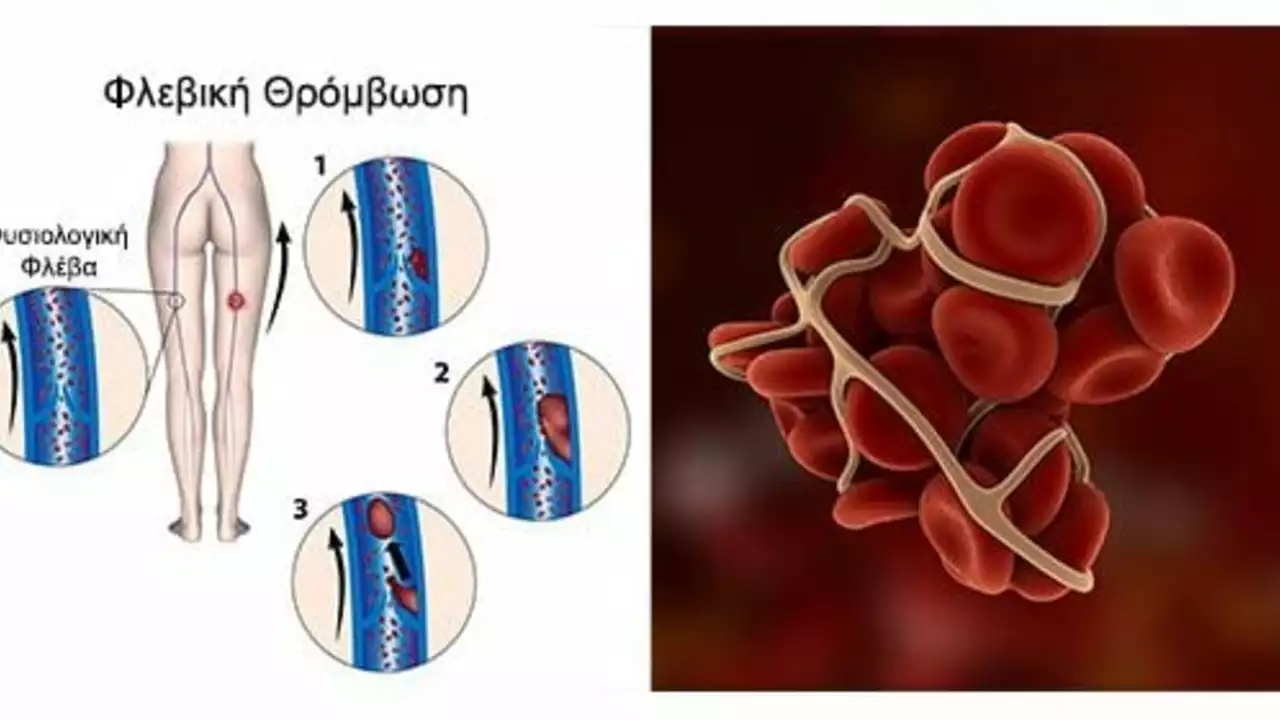
Ever had a sore, swollen calf and wondered if it’s just a muscle or something more dangerous? Deep vein thrombosis, or DVT, is a blood clot usually in the leg that can cause swelling, pain, and — if it breaks free — a life-threatening lung clot. Know the signs, act fast, and you lower the risk of serious problems.
How to spot DVT
Most DVTs happen in the calf or thigh. Look for one-sided swelling, warmth, redness, and a tender, aching feeling when you stand or walk. Sometimes you’ll only feel mild discomfort or nothing at all. If you suddenly get shortness of breath, sharp chest pain that gets worse when you breathe, or cough up blood, call emergency services — that could mean a pulmonary embolism (PE), which needs immediate care.
Doctors often use a duplex ultrasound to check for clots. A D-dimer blood test can help when the chance of DVT is low; it measures clot breakdown products. If results are unclear, your doctor may order CT or MRI scans.
Treatment and prevention
Treatment usually starts with blood thinners (anticoagulants). Common options include low-molecular-weight heparin, warfarin, and newer oral agents like apixaban or rivaroxaban. These drugs don’t break up the clot fast but stop it growing and lower the risk it will travel to the lungs. In rare cases, doctors use clot-busting medicines or place an IVC filter to protect the lungs.
Prevention is often simple and effective. If you’re on a long flight or car trip, stand up and walk every hour, flex your ankles and calves while seated, and drink water — avoid alcohol and heavy sleep aids. If you’re recovering from surgery or have a history of clots, your doctor may recommend compression stockings or short-term blood thinners.
Know your risk factors: recent surgery, long immobility, active cancer, pregnancy, obesity, smoking, certain hormone pills, and inherited clotting disorders. If you take birth control or hormone replacement therapy and have other risks, talk with your provider about safer options.
Managing long-term risk means staying active, keeping a healthy weight, quitting smoking, and controlling conditions like diabetes and high blood pressure. If you’ve had a DVT before, follow-up care and a plan for future trips or surgeries will help prevent recurrence.
If you suspect a DVT, don’t wait. Quick assessment and treatment reduce danger and improve outcomes. Ask questions: what anticoagulant is right for me, how long do I need it, and what side effects should I watch for? Your health team should give clear answers and a simple plan you can follow at home.
Keep this page bookmarked — small steps during travel or after surgery can make a big difference. If anything feels off, call your doctor. Better safe than sorry when it comes to blood clots.
Post-Thrombotic Syndrome: A Common Complication of Deep Vein Thrombosis
Well, folks, here we go! Post-Thrombotic Syndrome, or as I like to call it, "the annoying aftermath of Deep Vein Thrombosis." It's like that one guest who just doesn't know when to leave the party. Essentially, it's a common complication that may follow a bout of Deep Vein Thrombosis (DVT). It's a tricky little number, causing symptoms like pain, swelling, and skin changes in the affected limb. So, if you've had DVT, keep an eye out for this persistent party crasher!
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



