Medication-Related Bone Marrow Suppression: What You Need to Know About Low Blood Counts
Bone Marrow Suppression Assessment Tool
Blood Count Assessment
Enter your recent complete blood count (CBC) results to assess your bone marrow suppression risk. This tool uses clinical guidelines to help you understand your results.
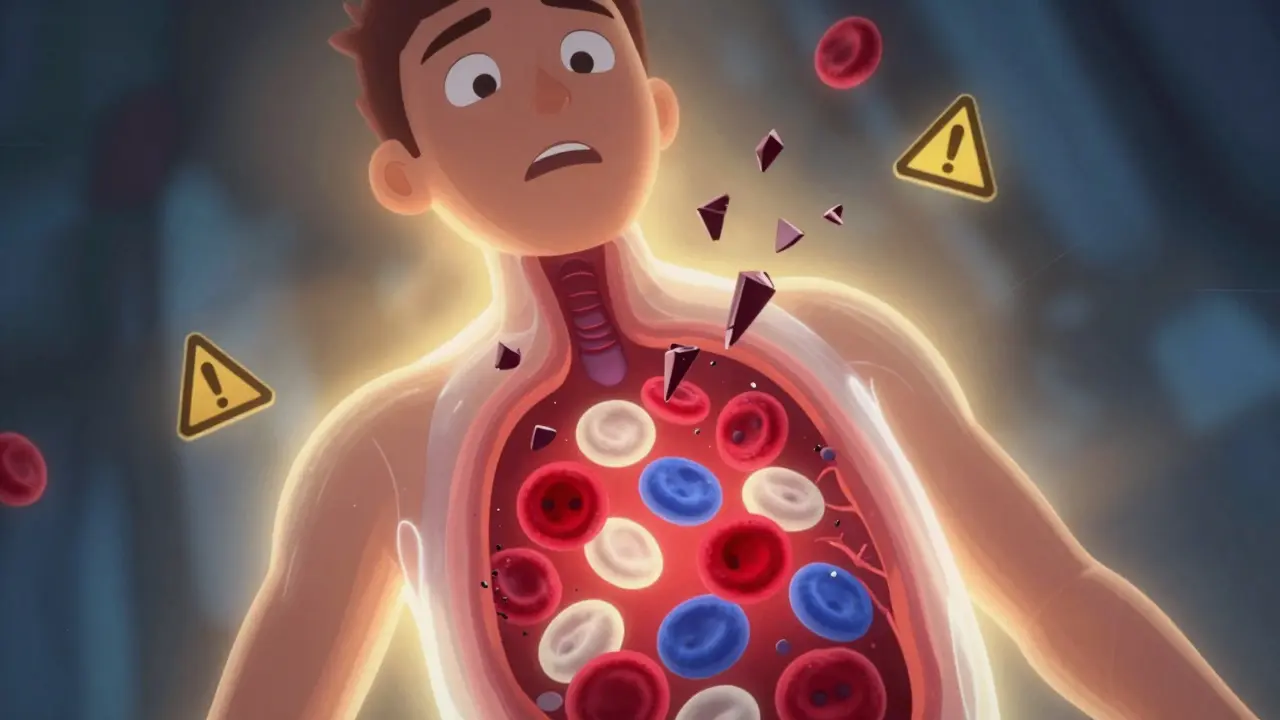
What Is Bone Marrow Suppression?
When your bone marrow slows down or stops making enough blood cells, it’s called bone marrow suppression. This isn’t just a minor side effect-it’s a serious drop in red blood cells, white blood cells, and platelets. Without enough red blood cells, you get tired and short of breath. Too few white blood cells mean you can’t fight off infections. Low platelets? That means you bruise easily or bleed for longer than normal.
This happens because certain medications-especially chemotherapy drugs-damage the stem cells in your bone marrow. These stem cells are supposed to grow into all the different types of blood cells your body needs. When they’re hit hard, your counts drop fast. The American Society of Hematology says 60% to 80% of people on chemotherapy experience this. It’s not rare. It’s expected.
How Do You Know If Your Blood Counts Are Low?
You won’t always feel it right away. But there are clear warning signs:
- Neutropenia: White blood cell count below 1,500 per microliter. You might get fevers, chills, or a sore throat that won’t go away. Even a mild cold can turn dangerous.
- Anemia: Hemoglobin under 13.5 g/dL for men or 12.0 g/dL for women. You’ll feel exhausted, dizzy, or pale. Your heart might race even when you’re sitting still.
- Thrombocytopenia: Platelets below 150,000 per microliter. You might notice tiny red dots on your skin (petechiae), nosebleeds, or bleeding gums. Severe cases drop below 50,000-then even a bump can cause big bruises.
These numbers aren’t guesses. They’re clinical standards set by the World Health Organization. Your doctor checks them with a simple blood test called a complete blood count, or CBC. Most oncology teams test you weekly during treatment. If your counts drop too low, they pause or adjust your meds.
Which Medications Cause This?
Chemotherapy is the biggest culprit. About 70% to 80% of bone marrow suppression cases come from chemo drugs like carboplatin, fludarabine, and doxorubicin. But it’s not just cancer drugs.
- Immunosuppressants: Azathioprine, used after organ transplants, causes suppression in 5% to 10% of patients.
- Antibiotics: Trimethoprim-sulfamethoxazole (Bactrim) can drop your counts, especially if you’re on it long-term.
- Antivirals and antiretrovirals: Some HIV meds, like zidovudine, are known to slow bone marrow activity.
- Anticonvulsants: Valproic acid and phenytoin can rarely cause this too.
It’s not about the drug alone-it’s about your body’s reaction. Some people take the same dose as someone else and stay fine. Others crash hard. That’s why monitoring is so critical.
When Does It Happen?
It doesn’t hit right away. Most people see their lowest blood counts-called the nadir-between 7 and 14 days after starting a new chemo cycle. That’s why doctors schedule blood tests around that window. For example, if you get carboplatin on Monday, your platelets might bottom out by the following Monday.
Some drugs are slower. Fludarabine can cause lymphocyte counts to stay low for months. Azathioprine might take weeks to show its effect. That’s why you can’t stop checking just because you feel okay.
How Is It Treated?
Treatment depends on how bad it is.
Grade 1-2 (mild): Your doctor might just watch. Maybe they lower your next dose. You’ll keep getting blood tests every week.
Grade 3-4 (severe): This is where things get urgent.
- Growth factors: Drugs like filgrastim (Neupogen) or pegfilgrastim (Neulasta) jump-start white blood cell production. Studies show they cut the time you’re neutropenic by over 3 days. But they’re expensive-up to $6,500 out of pocket in the U.S.
- Trilaciclib (CoSela): A newer option approved in 2021. Given before chemo, it protects bone marrow cells and reduces suppression by 47%. It’s only for small cell lung cancer patients right now, but research is expanding.
- Transfusions: If your hemoglobin drops below 8 g/dL, you’ll get red blood cell transfusions. Platelet transfusions kick in if counts fall below 10,000 or if you’re bleeding.
- Drug switches: If azathioprine is the problem, switching to mycophenolate mofetil helps restore counts in 78% of transplant patients within 6 weeks.
There’s no magic bullet. But the right mix of monitoring and medication can keep you on your treatment plan.
What Happens If You Don’t Manage It?
Ignoring low blood counts is dangerous.
Neutropenia can lead to neutropenic fever-a fever over 101°F with low white cells. That’s a medical emergency. Infections can spread fast. One study showed 1 in 5 cancer patients with untreated neutropenia ended up in the ICU.
Severe anemia can strain your heart. Platelet counts below 10,000 can cause internal bleeding. In rare cases, bone marrow suppression becomes permanent. That’s when doctors consider a stem cell transplant. Success rates? 65% to 75% with a matched sibling donor.
And it’s not just physical. A 2022 survey found 74% of cancer patients had treatment delayed because of low counts. Nearly half stopped treatment altogether. That means the drug meant to save you might end up stopping your cure.

What Can You Do?
You can’t control the drug, but you can control how you respond.
- Check your temperature daily. Any fever above 101°F? Call your oncologist immediately.
- Avoid crowds and sick people. Wash your hands often. Skip restaurants during outbreaks.
- Use a soft toothbrush. No flossing if platelets are low. Bleeding gums are a red flag.
- Don’t take NSAIDs. Ibuprofen and aspirin can thin your blood. Use acetaminophen instead, unless your doctor says otherwise.
- Track your symptoms. Write down fatigue, bruising, or infections. Bring it to every appointment.
Some hospitals now use predictive tests. A lab test called a colony-forming assay can predict your risk of severe suppression before you even start chemo. It’s not everywhere yet-but ask your doctor if it’s available.
What’s New in 2026?
The field is moving fast.
In 2023, the FDA approved lixivaptan to reduce transfusion needs by 31%. Magrolimab, an experimental drug, cut anemia in myelodysplastic syndrome patients by over half in early trials.
Genetics is changing the game. People with TP53 mutations are 3.7 times more likely to have severe suppression. That means in the next few years, doctors might test your DNA before starting chemo-and pick drugs that won’t wreck your bone marrow.
And the market is growing. The global bone marrow protection market hit $9.8 billion in 2022. By 2027, it’s expected to hit $14.3 billion. That’s because more people are surviving cancer-and living long enough to need better ways to handle side effects.
Final Thoughts
Bone marrow suppression isn’t a sign that treatment is failing. It’s a sign that the treatment is working-too well. The drugs are killing cancer cells, but they’re also hitting your healthy ones.
The goal isn’t to avoid it. It’s to manage it. With smart monitoring, timely interventions, and open communication with your care team, you can stay on track. You don’t have to choose between beating cancer and staying healthy. The tools are here. You just need to use them.
Can bone marrow suppression be permanent?
In most cases, bone marrow suppression is temporary and reverses once the medication is stopped or the dose is adjusted. However, in rare cases-especially with prolonged exposure to certain drugs like chemotherapy or radiation-bone marrow can become permanently damaged. This is more common in older adults or those with pre-existing bone marrow conditions. If counts don’t recover after stopping the drug, a bone marrow biopsy and possible stem cell transplant may be needed.
How often should I get blood tests during chemotherapy?
Most oncology teams test your complete blood count (CBC) at least once a week during active chemotherapy cycles. For high-risk drugs like carboplatin or fludarabine, testing may occur every 3 to 4 days around days 7 to 14, when counts typically hit their lowest point. Pediatric protocols often require even more frequent checks, sometimes every 48 hours. Always follow your care team’s schedule-don’t skip tests just because you feel fine.
Are there natural ways to boost blood counts during suppression?
No supplement, herb, or diet can reliably raise your blood counts when bone marrow suppression is caused by medication. While good nutrition supports overall health, it doesn’t replace the need for medical interventions like growth factors or transfusions. Some patients try iron, B12, or folic acid-but these only help if you’re deficient. In drug-induced suppression, the problem is your bone marrow, not your diet. Always talk to your doctor before taking anything new.
Why do some people get bone marrow suppression and others don’t?
It depends on genetics, age, overall health, and the specific drug and dose. For example, people with TP53 gene mutations are nearly 4 times more likely to have severe suppression. Older adults, those with prior chemo exposure, or those with kidney or liver disease are also at higher risk. Even small differences in how your body metabolizes drugs can make a big difference. That’s why personalized medicine is becoming so important-your treatment should be tailored to your biology, not just your diagnosis.
Can I still work or go out in public if I have low blood counts?
It depends on how low your counts are. If your neutrophil count is below 1,000, you’re at high risk for infection. Avoid crowded places, public transit during rush hour, and sick people. Working from home is often the safest option. If your platelets are below 50,000, avoid contact sports, heavy lifting, or anything that could cause injury. Your care team will give you specific guidance based on your numbers. When in doubt, err on the side of caution.
Is bone marrow suppression the same as leukemia?
No. Bone marrow suppression is a side effect of medication that temporarily reduces blood cell production. Leukemia is a cancer of the blood and bone marrow where abnormal cells multiply uncontrollably. While some chemotherapy drugs can rarely lead to secondary leukemia years later, suppression itself is not cancer. The confusion comes because both involve low blood counts-but the causes and treatments are completely different.
What should I do if I develop a fever while my counts are low?
Call your oncologist or go to the emergency room immediately. A fever over 101°F with low neutrophils is called neutropenic fever-and it’s a medical emergency. Even if you feel fine otherwise, an infection can spread rapidly. Do not wait. Do not take antibiotics you have at home. You’ll likely need IV antibiotics in the hospital. Delaying treatment increases your risk of sepsis and death.




Rachel Kipps
February 2, 2026 AT 22:19Went to the ER last night because I felt a little warm, and they said my neutrophils were at 800. They gave me antibiotics and told me to call my oncologist first next time. I'm so tired of being scared all the time.
Wendy Lamb
February 3, 2026 AT 00:54And yes, fever = ER. No exceptions.
Justin Fauth
February 3, 2026 AT 19:11Amit Jain
February 5, 2026 AT 00:58rahulkumar maurya
February 5, 2026 AT 02:27Jamillah Rodriguez
February 6, 2026 AT 07:16Susheel Sharma
February 7, 2026 AT 19:55Janice Williams
February 8, 2026 AT 13:46Roshan Gudhe
February 9, 2026 AT 23:04Prajwal Manjunath Shanthappa
February 10, 2026 AT 17:57Antwonette Robinson
February 11, 2026 AT 11:44Ed Mackey
February 12, 2026 AT 03:16Also, my doc said 'just avoid NSAIDs' but didn't say what to use instead. So I'm just taking Tylenol but I don't know if that's right. Sorry for the typos-typing with numb fingers is hard.