Lamivudine (Epivir HBV) vs Other Hepatitis B Antivirals: A Practical Comparison

HBV Antiviral Comparison Tool
This tool helps compare key attributes of Lamivudine and other hepatitis B antivirals:
| Drug | Class | Resistance Rate (5 yr) | Renal Impact | Typical Cost (CAD / mo) |
|---|---|---|---|---|
| Lamivudine | Nucleoside analogue | ≈30 % | None | ≈15 |
| Tenofovir disoproxil fumarate (TDF) | Nucleotide analogue | ≈1 % | Moderate | ≈40-50 |
| Entecavir | Guanosine analogue | ≈1 % | Minimal | ≈70-90 |
| Adefovir dipivoxil | Nucleotide analogue | ≈2-3 % | High | ≈40-50 |
| Tenofovir alafenamide (TAF) | Nucleotide analogue | ≈1 % | Low | ≈70-90 |
Quick Summary:
- Resistance: Lamivudine has the highest resistance risk (~30%) after 5 years; others have less than 1%.
- Renal Impact: TDF and Adefovir pose higher risks; TAF and Lamivudine have minimal impact.
- Cost: Lamivudine is the cheapest (~CAD 15/month); TAF and Entecavir are pricier (~CAD 70-90/month).
Epivir HBV (Lamivudine) is a nucleoside analogue antiviral approved for chronic hepatitis B infection, introduced in 1998, with a standard dose of 100mg once daily. It works by inhibiting the viral DNA polymerase and has a favorable safety record, but resistance can emerge after long‑term use.
Why Lamivudine Still Shows Up in Guidelines
Lamivudine earned a place in early HBV treatment guidelines because it is inexpensive, easy to take, and has minimal renal toxicity. In Canada, public drug plans often list it as a first‑line option for patients with low baseline viral load or those who cannot tolerate tenofovir.
Key Players in the HBV Antiviral Landscape
Beyond Lamivudine, clinicians rely on a handful of newer nucleos(t)ide analogues. The most common alternatives are:
- Tenofovir disoproxil fumarate (TDF) - a nucleotide analogue with a high barrier to resistance, approved in 2001.
- Entecavir - a guanosine analogue introduced in 2005, also known for low resistance rates.
- Adefovir dipivoxil - a weaker nucleotide analogue, launched in 2002, useful in cases of TDF intolerance.
- Tenofovir alafenamide (TAF) - a newer pro‑drug of tenofovir with reduced bone and kidney impact, approved in 2016.
All of these agents belong to the broader class of nucleos(t)ide analogues - synthetic compounds that mimic the natural building blocks of viral DNA and cause chain termination.
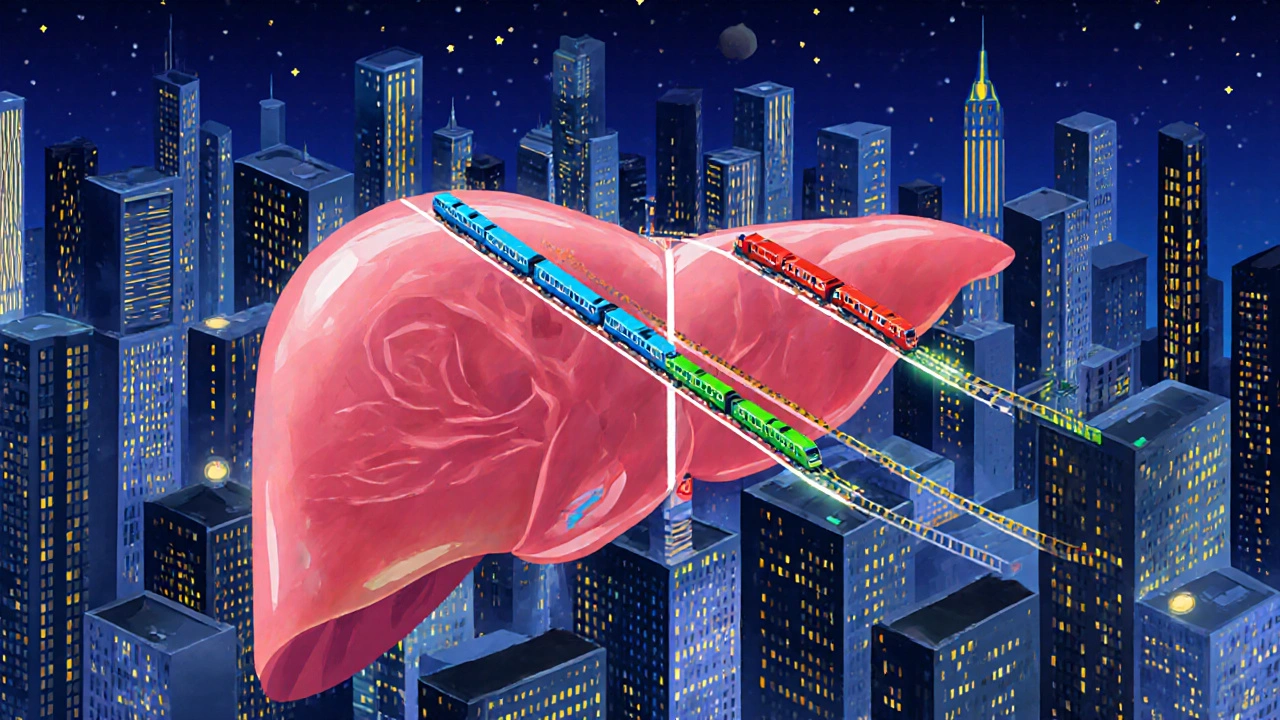
How They Work - A Quick Mechanistic Snapshot
Each drug interferes with the hepatitis B virus (HBV) polymerase in a slightly different way. Lamivudine and Entecavir are true nucleosides, needing intracellular phosphorylation before they become active. Tenofovir (both TDF and TAF) and Adefovir are nucleotides, already carrying a phosphate group, which speeds up activation and contributes to their higher potency.
Resistance - The Real Deal
Resistance is the Achilles’ heel of chronic HBV therapy. Lamivudine’s low genetic barrier means mutations (M204V/I) can appear after 1‑2 years in up to 30% of patients. In contrast, Entecavir and tenofovir variants require multiple concurrent mutations, keeping resistance below 1% even after five years of treatment. Adefovir sits somewhere in the middle, with a reported 2‑3% resistance rate after four years.
Safety and Tolerability Profiles
All agents are generally well‑tolerated, but their side‑effect fingerprints differ:
- Lamivudine - minimal impact on kidneys or bones; occasional headache or fatigue.
- Tenofovir disoproxil fumarate - rare cases of proximal renal tubulopathy and modest bone mineral density loss, especially in older adults.
- Tenofovir alafenamide - similar antiviral strength as TDF but with far less renal and skeletal toxicity.
- Entecavir - rarely causes lactic acidosis; safe for most patients with normal renal function.
- Adefovir - higher dose (30mg) linked to dose‑related nephrotoxicity; low‑dose (10mg) is safer but less potent.
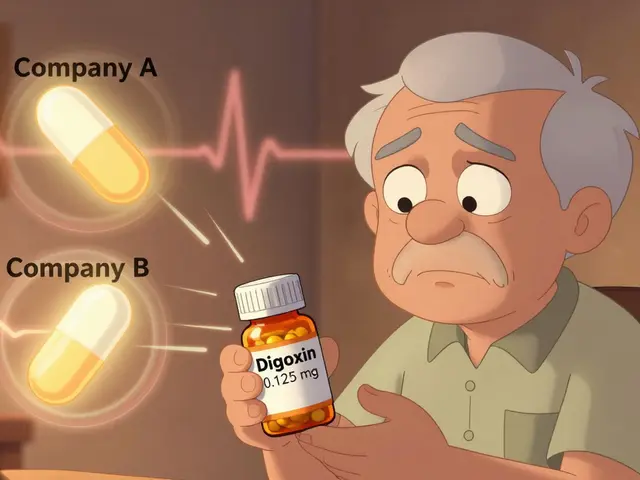
Cost Considerations in Canada
Price can be a deciding factor for many. Generic lamivudine typically costs under CAD15 per month, making it the most affordable option on provincial formularies. Tenofovir disoproxil fumarate’s generic version runs around CAD40‑50 monthly, while TAF and Entecavir sit in the CAD70‑90 range, reflecting their newer patents.
Side‑by‑Side Comparison Table
| Drug | Class | Resistance Rate (5yr) | Renal Impact | Typical Cost (CAD/mo) |
|---|---|---|---|---|
| Lamivudine | Nucleoside analogue | ≈30% | None | ≈15 |
| Tenofovir disoproxil fumarate (TDF) | Nucleotide analogue | <1% | Low‑to‑moderate (monitor eGFR) | ≈45 |
| Entecavir | Nucleoside analogue | <1% | None | ≈80 |
| Adefovir dipivoxil | Nucleotide analogue | 2‑3% | Potential nephrotoxicity at 30mg | ≈30 |
| Tenofovir alafenamide (TAF) | Nucleotide analogue (pro‑drug) | <1% | Minimal | ≈90 |
When to Pick Lamivudine
If a patient needs an ultra‑low‑cost option, has well‑controlled renal function, and is unlikely to stay on therapy for many years (e.g., short‑term suppression before liver transplantation), lamivudine makes sense. It also fits pediatric dosing schedules, as the 2‑mg/kg rule is straightforward.
When to Reach for a Higher‑Barrier Agent
For anyone with a high baseline viral load (>10⁷IU/mL), evidence of liver fibrosis (F2‑F4), or a history of lamivudine‑resistant mutations, tenofovir (TDF or TAF) or entecavir are preferred. Those with pre‑existing kidney disease should lean toward entecavir or TAF, which spare the kidneys.
Practical Switching Strategies
Switching from lamivudine to a higher‑barrier drug is common once resistance appears. The recommended approach is:
- Confirm resistance with a genotype test (M204V/I).
- Initiate tenofovir (or entecavir) without a washout period.
- Continue lamivudine for 2-4 weeks only if the patient has baseline HBV DNA>10⁶IU/mL, to avoid a viral rebound.
- Discontinue lamivudine permanently once the new drug reaches steady‑state (usually 2 weeks).
Patients should have liver enzymes checked at weeks 4, 12, and then every 6 months.
Related Concepts Worth Knowing
Understanding the broader context helps clinicians and patients make smarter choices. Key related topics include:
- Chronic hepatitis B - the underlying disease state, often silent until cirrhosis develops.
- Liver fibrosis staging - assessed by elastography; guides urgency of treatment.
- HBV DNA viral load - the primary marker of treatment response.
- Antiviral adherence - even the best drug fails if doses are missed.
- Pregnancy considerations - lamivudine is Category B, while tenofovir is also safe, making both options viable for expectant mothers.
Bottom Line for the Busy Reader
Lamivudine remains a viable, cheap option for low‑risk patients, but its high resistance rate limits long‑term use. Newer agents-especially tenofovir (TDF/TAF) and entecavir-offer stronger viral suppression and a near‑zero resistance ceiling, at a modest price premium. The choice should balance cost, kidney health, viral load, and how long therapy is expected to continue.
Frequently Asked Questions
Can I use Lamivudine if I have mild kidney disease?
Yes. Lamivudine is cleared mainly by the liver, so it does not require dose adjustment in mild to moderate renal impairment. However, if you expect to stay on therapy for many years, discuss a switch to a higher‑barrier drug to avoid resistance.
How quickly does resistance to Lamivudine develop?
Mutations typically appear after 12‑24 months of continuous therapy. In population studies, roughly 30% of patients develop the M204V/I mutation within five years.
Is Tenofovir alafenamide (TAF) safer for my bones than Tenofovir disoproxil fumarate (TDF)?
Clinical trials show TAF causes only a 1‑2% decrease in bone mineral density versus a 3‑5% decline with TDF after two years. For patients over 50 or those with osteoporosis risk, TAF is the preferred option.
Do I need to stop Lamivudine before starting Entecavir?
No washout is required. Entecavir can be added directly while continuing lamivudine for a short overlap period (2‑4 weeks) to prevent a transient viral spike, then lamivudine is discontinued.
Which HBV drug is best for a pregnant woman?
Both lamivudine and tenofovir are classified as pregnancy‑category B and have extensive safety data. Choice usually hinges on the mother’s renal function and whether she already has resistance to lamivudine.




leo dwi putra
September 27, 2025 AT 13:49Oh, the saga of lamivudine versus the shiny new tenofovir… it's like watching a low‑budget indie film battling a blockbuster sequel! While the cheap price tag (≈CAD 15/month) sings a lullaby to budget‑conscious patients, the 30 % resistance after five years sneaks in like an uninvited plot twist. Imagine prescribing a drug that whispers “I’m safe for kidneys” while secretly plotting mutational fireworks. The renal innocence is commendable, but the high‑risk resistance is the real villain draped in a hero’s cape. In the grand theater of HBV therapy, lamivudine gets a standing ovation for affordability, yet the applause fades when the virus learns to dodge its move. If your clinic loves drama, let the resistance data be the cliffhanger that keeps you on edge.
-
Krista Evans
October 6, 2025 AT 11:46Hey folks, if you’re weighing cost against long‑term success, think of lamivudine as the friendly starter bike-easy to hop on and cheap to keep running. It’s great for patients who need a gentle entry point, especially when kidney health is a concern. Just keep an eye on those resistance numbers and have a backup plan ready. You’ve got this, and there are plenty of options if the virus decides to switch teams!
Mike Gilmer2
October 15, 2025 AT 09:42Alright, let’s cut to the chase-lamivudine is the classic underdog that still shows up at the party, cheap as chips but with a nasty surprise up its sleeve. Resistance? Yeah, roughly 30 % after half a decade, so it’s like inviting a guest who forgets to bring the dessert and then disappears. Tenofovir and entecavir wear the armor of low‑resistance, but they’ll make your wallet weep. In short, pick your fighter: low‑cost zero‑renal‑impact but watch the mutational fireworks, or splurge for the big guns and keep the kidneys happy.
Alexia Rozendo
October 24, 2025 AT 07:39Well, isn’t lamivudine just the budget superhero we all needed? Saves you a fortune, spares your kidneys, and then-boom-throws a 30 % resistance curveball like it’s a surprise party. If you love living on the edge, go ahead, but don’t be surprised when the virus decides it’s time for a plot twist. Congrats on finding the “cheapest” option, enjoy the dramatic sequel.
Snehal Suhane
November 2, 2025 AT 04:36Oh dear, the masses still clutch at lamivudine like it’s a vintage vinyl in a world of streaming. Sure, it’s under CAD 15 a month-prix d’entrée for the financially challenged-but its 30 % resistance rate is practically an invitation to viral rebellion. One might argue that paying extra for TDF or TAF is the hallmark of a discerning clinician, not a penny‑pinching dilettante. In any case, the low renal toxicity is the only redeeming virtue, albeit a modest one. So if you’re content with mediocrity, lamivudine will serve as your trusty sidekick.
Ernie Rogers
November 11, 2025 AT 02:32Look guys lamivudine is cheap and easy but yeah the resistance rate is high. If you want something that actually works long term maybe look at tenofovir or entecavir they cost more but do the job better less kidney issues.
nathaniel stewart
November 20, 2025 AT 00:29Esteemed colleagues, it is with great optimism that I highlight lamivudine’s unique position in the therapeutic armamentarium. Its modest expense, approximately CAD 15 per month, renders it accessible to a broad patient demographic. While the resistance incidence approaches 30 % over five years, diligent monitoring and timely regimen adjustment can mitigate adverse outcomes. Moreover, its negligible impact on renal function affirms its safety profile. In sum, lamivudine offers a viable, cost‑effective foundation upon which personalized treatment strategies may be constructed, provided clinicians remain vigilant.
Pathan Jahidkhan
November 28, 2025 AT 22:26Life is a cascade of nucleotides and lamivudine sits at the edge of this river watching the currents of resistance swirl around it. It whispers cheap promises while the virus laughs quietly. No kidneys hurt, sure, but the mutational storm after years is a reminder that cheap thrills fade fast. In the grand scheme, perhaps we need not chase the cheap mirage but seek the deeper safety of tenofovir or entecavir. The choice, like all choices, is a silent echo in the molecular abyss.
Dustin Hardage
December 7, 2025 AT 20:22From a mechanistic perspective, lamivudine functions as a nucleoside analogue that requires intracellular phosphorylation to become active against HBV polymerase. Its low cost (≈CAD 15/month) and minimal renal toxicity are advantageous in settings with limited resources or patients with pre‑existing renal impairment. However, the relatively low genetic barrier to resistance-approximately 30 % after five years-necessitates careful virologic monitoring. Alternative agents such as tenofovir disoproxil fumarate (TDF) or entecavir possess higher barriers to resistance (≤1 %) and comparable safety profiles, albeit at higher monthly costs (CAD 40–90). Clinicians should therefore balance pharmacoeconomic considerations with long‑term efficacy and resistance risk when selecting an antiviral regimen.
Dawson Turcott
December 16, 2025 AT 18:19Lamivudine saves you cash but the virus might dump you later 😂
Alex Jhonson
December 25, 2025 AT 16:16Hey everyone, just a heads‑up that while lamivudine’s price tag is the friendliest on the block, the 30 % resistance rate is something to keep on your radar. If you’re working with diverse populations, consider the trade‑off between affordability and the potential need for a switch later on. A proactive approach-regular viral load checks and patient education-can smooth the journey, no matter which drug you start with.
Leslie Woods
January 3, 2026 AT 14:12Lamivudine’s low renal impact makes it a solid option for patients with kidney concerns while keeping costs down
Manish Singh
January 12, 2026 AT 12:09Understanding that some patients may be worried about the higher resistance of lamivudine, it helps to reassure them that close monitoring and open communication can catch any viral breakthrough early, allowing a timely transition to a more robust therapy if needed.
Dipak Pawar
January 21, 2026 AT 10:06When we examine the pharmacoeconomic landscape of chronic hepatitis B management, lamivudine emerges as a paradigmatic example of cost‑efficiency juxtaposed against virologic durability. Its molecular architecture as a nucleoside analogue confers a favorable safety profile, particularly the absence of nephrotoxic sequelae, which is highly pertinent in patient cohorts with comorbid chronic kidney disease. Nonetheless, the epidemiological data underscore a resistance incidence approximating thirty percent after a quinquennial horizon, reflecting a relatively low genetic barrier attributable to the M204V/I polymerase mutations. This mutational propensity translates into a clinical conundrum wherein the initial fiscal advantage may be offset by downstream costs associated with resistance testing, regimen escalation, and potential hepatic decompensation. Conversely, agents such as tenofovir disoproxil fumarate and entecavir exhibit resistance rates at or below one percent, attributable to their higher genetic thresholds requiring multiple concurrent mutations for virologic escape. The pharmacokinetic attributes of tenofovir, particularly its pro‑drug formulation, facilitate intracellular delivery of tenofovir diphosphate, thereby enhancing antiviral potency while modulating renal toxicity through dose optimization. Yet, the expense associated with tenofovir analogues, often ranging from CAD 40 to 90 per month, imposes a substantial budgetary impact on health systems and out‑of‑pocket patients alike. In resource‑constrained settings, the decision matrix must therefore integrate variables such as drug acquisition cost, projected adherence, baseline viral load, and the prevalence of pre‑existing resistance mutations. Moreover, the evolving evidence base for tenofovir alafenamide, with its attenuated bone and renal safety concerns, introduces an additional layer of therapeutic nuance, albeit at a premium price point reflective of its novel formulation. Ultimately, the selection of lamivudine versus alternative nucleos(t)ide analogues should be predicated upon a comprehensive assessment of patient‑specific factors, longitudinal risk stratification, and the fiscal realities of the prescribing institution. By employing a multidisciplinary approach that synergizes hepatology expertise, pharmacoeconomic analysis, and patient education, clinicians can navigate the intricate trade‑offs inherent to HBV antiviral therapy and optimize long‑term outcomes.
Jonathan Alvarenga
January 30, 2026 AT 08:02Reading this comparison feels like watching a marketing brochure masquerading as scientific analysis. The table reduces complex pharmacodynamics to a few bland numbers, ignoring real‑world adherence challenges and the nuanced toxicity profiles that clinicians grapple with daily. Lamivudine’s cheap price is hailed as a virtue, yet the author conveniently downplays the clinical ramifications of a thirty‑percent resistance rate, which can precipitate treatment failure and costly rescue therapy. Meanwhile, the discussion of tenofovir’s renal impact lacks depth, glossing over the spectrum of proximal tubular dysfunction reported in vulnerable populations. The narrative would have benefited from a more rigorous meta‑analysis, inclusion of head‑to‑head trial data, and consideration of patient‑reported outcomes. As it stands, the piece offers a superficial snapshot that could mislead prescribers who rely solely on cost rather than a holistic assessment of efficacy, safety, and long‑term sustainability.
Jim McDermott
February 8, 2026 AT 05:59Just wanted to add that for patients who are already on lamivudine and doing well, there's no need to switch unless you see rising viral loads or signs of resistance. Keep an eye on their labs and talk to them about any side effects-most folks tolerate it great. If you do need to change, tenofovir or entecavir are solid next steps, even though they're pricier.
Naomi Ho
February 17, 2026 AT 03:56Lamivudine offers a low‑cost, low‑renal‑impact option but its high resistance risk means regular monitoring is essential