Insurance Coverage of Generic Combinations vs Individual Generics: What You Pay and Why
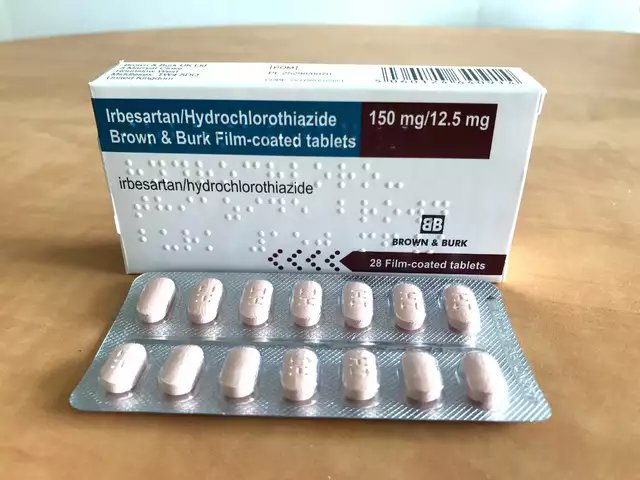
When your doctor prescribes a medication for high blood pressure, diabetes, or cholesterol, you might get a single pill with two active ingredients - a generic combination. Or you might get two separate pills, each with one ingredient - individual generics. At first glance, they seem the same. But your insurance plan might treat them very differently - and that can change your monthly bill by hundreds of dollars.
Why Insurance Plans Care About Combination Pills
Insurance companies don’t just pick drugs randomly. They build formularies - lists of covered medications - based on cost, effectiveness, and how likely patients are to take them correctly. Generic combination pills are designed to simplify treatment. One pill instead of two means fewer chances of missing a dose. That’s good for your health. But for insurers, it’s also about controlling costs. In 2019, 84% of Medicare Part D plans covered only generic drugs, not brand-name ones. That number has been climbing since 2012. Why? Because generics cost 80-85% less than brand-name drugs. When six or more companies make the same generic, prices can drop by up to 95%. That’s a huge savings for insurers. So they push generics hard. But here’s the twist: a combination pill might be priced higher than the two individual generics - even if it’s the exact same ingredients. Why? Because the combination version might be a single-source generic. That means only one manufacturer makes it. No competition. No price war. So the insurer puts it on a higher tier, making you pay more.How Medicare and Private Plans Handle Generics
Medicare Part D plans use a four-tier system:- Tier 1: Preferred generics - often $0-$5 copay
- Tier 2: Preferred brand-name drugs - $10-$40
- Tier 3: Non-preferred brand-name drugs - $40-$80
- Tier 4: Specialty drugs - $100+
The Real Cost Difference: Stories from Patients
One patient on Reddit shared: “My plan covers the two individual generics for $10 each. The combo pill? $50. I had to ask my doctor to write two separate prescriptions just to save money.” Another patient said: “My blood pressure combo went generic. My copay dropped from $45 to $7. No side effects. Same results. I didn’t even notice the change.” The difference isn’t just about price - it’s about predictability. When you’re on a fixed income, a $50 copay can mean skipping groceries. A $7 copay means you can afford your meds without choosing between them and your rent. The key? It’s not about the drug - it’s about how your plan structures coverage.
Why Some Combination Pills Are More Expensive
Not all combination drugs are created equal. If a brand-name combo like Exforge (amlodipine + valsartan) goes generic, the generic version might be priced lower than the brand - but still higher than the two separate generics. Why? Because the manufacturer of the generic combo might be the only one approved to make it. No competition. No pressure to lower prices. This is called a single-source generic. These are rare, but they exist - especially for newer combinations. Compare that to a drug like metformin, which has over 50 generic manufacturers. Price? $3 a month. That’s the power of competition. So if your combo drug costs more than the sum of its parts, ask your pharmacist: “Is this a single-source generic?” If yes, you might be better off splitting it.What You Can Do to Save Money
You don’t have to accept whatever your plan says. Here’s how to fight back:- Check your plan’s formulary. Go to your insurer’s website and search for your drug by name. Look at the tier and copay for both the combo and the individual drugs.
- Ask your doctor to write separate prescriptions. If the individual generics are cheaper, your doctor can prescribe them as two separate meds. Most insurers allow this - as long as they’re medically appropriate.
- Use the Medicare Plan Finder. If you’re on Medicare, use the official tool to compare plans. You can filter by drug coverage and see exactly how much you’ll pay for each option.
- Request a coverage determination. If your plan denies the combo but you need it, your doctor can file a formal appeal. It takes 72 hours for a standard request, 24 hours if you’re in danger.
- Check for manufacturer coupons. Even for generics, some companies offer savings cards. The 2023 court ruling against copay accumulators means those discounts now count toward your out-of-pocket max.

What’s Changing in 2025
Starting in 2024, the Inflation Reduction Act capped Medicare Part D out-of-pocket costs at $2,000 per year. That’s huge. But it also means insurers are adjusting their formularies to push the cheapest options first - which usually means individual generics over combo pills. Also, the FDA’s Generic Drug User Fee Amendments (GDUFA) III are speeding up approvals. More generic combos are coming. By 2028, the FDA expects 93% of prescriptions to be generics - up from 90% today. That means more competition, lower prices, and better coverage for combination drugs. But until then, you need to be proactive. Don’t assume the combo is the best deal. Always compare.When to Stick With the Combo
There are times when the combo pill is the better choice:- You have trouble remembering to take two pills a day.
- You’re on a complex regimen and simplifying helps you stay on track.
- The combo is the only generic version available - and it’s priced lower than buying two separate generics.
Bottom Line: Know Your Plan, Ask Questions
Insurance coverage for generic combinations isn’t about right or wrong. It’s about structure - and structure can work for you or against you. The bottom line? Always compare the cost of the combination pill versus the individual generics. Your pharmacist can run the numbers in seconds. Your doctor can adjust your prescription. And your insurer has to give you a clear explanation if they deny coverage. You’re not just a patient. You’re a consumer. And you have the right to know what you’re paying for - and why.Are generic combination drugs as safe as individual generics?
Yes. The FDA requires generic combination drugs to be bioequivalent to their brand-name counterparts - meaning they work the same way in your body. The active ingredients, dosage, strength, and how they’re absorbed are identical. The only differences might be in inactive ingredients like fillers or coatings, which rarely affect safety or effectiveness.
Why does my insurance cover the two separate pills but not the combo?
It’s usually about cost. If the two individual generics are cheaper together than the combo pill - even if they’re the same ingredients - your insurer will prefer them. This often happens when the combo is a single-source generic with no competition, making it more expensive than the sum of its parts. Insurers design formularies to steer patients toward the lowest-cost option.
Can I ask my doctor to prescribe individual generics instead of a combo?
Absolutely. Many doctors will do this if it saves you money and is medically appropriate. You don’t need a special reason - just ask. Your doctor can write two prescriptions, one for each generic. Most insurers allow this, and it’s a common way to reduce out-of-pocket costs.
What is a single-source generic?
A single-source generic is a generic drug made by only one manufacturer. Without competition, prices don’t drop as much. These are common with newer generic combos or drugs that are hard to manufacture. They can be priced closer to brand-name drugs, which is why insurers sometimes put them on higher tiers.
How do I find out what my insurance plan covers?
Log in to your insurer’s website and use their drug formulary tool. Search for your medication by name. You’ll see the tier, copay, and whether prior authorization is needed. If you’re on Medicare, use the Medicare Plan Finder. You can also call your pharmacy - they have real-time access to your plan’s coverage rules.
Will the Inflation Reduction Act make generic combos cheaper?
It won’t directly lower prices, but it will reduce your out-of-pocket costs. Starting in 2024, Medicare Part D patients pay no more than $2,000 a year for all drugs, regardless of tier. This gives you more room to choose the combo if it’s better for you, even if it’s slightly more expensive. It also means manufacturer coupons now count toward your cap, making savings programs more valuable.
What if my plan denies coverage for the combo I need?
You can file a coverage determination request. Your doctor must submit a letter explaining why the combo is medically necessary - for example, if you’ve had side effects from the individual drugs or have trouble taking multiple pills. The plan has 72 hours to respond. If denied, you can appeal. Expedited reviews are available if your health is at risk.





Benjamin Glover
December 15, 2025 AT 21:29Combination pills? More like corporate greed wrapped in a pillbox. If you’re dumb enough to take one without checking the tier, you deserve to pay $50.
RONALD Randolph
December 15, 2025 AT 23:55Let’s be crystal-clear: insurance formularies are not designed to help you-they’re engineered to maximize profit margins. If your combo pill is priced higher than the sum of its parts, it’s because the manufacturer holds a monopoly. And that’s not a bug-it’s a feature. The FDA approves these single-source generics, but Congress doesn’t regulate pricing. So yes, you’re being gouged. And no, your doctor isn’t going to fix it. You have to fight.
Check your plan’s formulary. Every. Single. Time. Use the Medicare Plan Finder. Call your pharmacy. Demand a breakdown. If they say “it’s covered,” ask: “At what tier? What’s the copay for the individual generics?” If they hesitate, they’re hiding something. This isn’t healthcare-it’s a marketplace. And you’re the customer. Act like it.
And don’t get me started on “step therapy.” That’s just bureaucratic torture dressed up as cost control. You’re not a lab rat. You’re not a spreadsheet. You’re a human being trying to stay alive. If your doctor says the combo is better for adherence, fight for it. File a prior auth. Appeal. Do it. Because if you don’t, someone else will profit from your compliance.
The Inflation Reduction Act caps your out-of-pocket at $2,000? Great. But that doesn’t change the fact that your copay for the combo is still $50. That’s $43 more than you should be paying. And that’s money you could use for food, heat, or gas. This isn’t about “choice.” It’s about exploitation. And if you’re not screaming about it, you’re part of the problem.
Stop trusting the system. Start auditing your prescriptions.
Raj Kumar
December 17, 2025 AT 19:50Bro, I get it-insurance is wild. But here’s the thing: in India, we don’t even have this problem. Generic combos are dirt cheap because 10 companies make them. Like, metformin + glibenclamide? Like $2 a month. No tier system, no prior auth. Just buy it at the local chemist. So when I see folks in the US paying $50 for the same combo? My heart breaks. You’re not alone. Talk to your pharmacist. Ask if they can order the individual generics in bulk. Sometimes they can. And don’t be shy-pharmacists love helping people save money. Seriously, they’re the real MVPs.
John Brown
December 19, 2025 AT 09:11Just wanted to say-this post saved me $400 last month. I was on a combo pill that cost $55. My pharmacist pulled up the individual generics-both were $8 each. I asked my doctor to switch. Done. No drama. No drama. My BP is the same. I’m sleeping better because I’m not stressing about bills. If you’re on meds, do this. It’s not hard. You’ve got rights.
Christina Bischof
December 19, 2025 AT 23:58My grandma takes three pills a day and forgets half of them. The combo saved her life. I’m glad some people can save money, but don’t shame others for needing simplicity. Health isn’t a spreadsheet.
Jocelyn Lachapelle
December 21, 2025 AT 11:18Just got my new plan details and my combo went from $45 to $7. I cried. Not because I’m emotional-I’m just tired of choosing between meds and groceries. Thank you for writing this. You made me feel less alone.
John Samuel
December 22, 2025 AT 09:56It is of paramount importance to underscore that the structural inequities embedded within the pharmaceutical reimbursement paradigm are not merely fiscal anomalies-they are systemic manifestations of market failure. The absence of competitive dynamics in the single-source generic market constitutes a violation of the fundamental tenets of economic efficiency. One must, therefore, advocate for legislative intervention to mandate multi-source approval thresholds for combination generics, thereby restoring price elasticity and patient autonomy. Furthermore, the utilization of manufacturer coupons, now cognizant of the 2023 copay accumulator ruling, represents a tactical triumph of consumer agency within a hostile regulatory landscape. One is reminded that the Hippocratic Oath does not extend to corporate shareholders.
Sai Nguyen
December 23, 2025 AT 10:22USA is broken. In my country, we don’t let pharma companies charge $50 for two pills. You people are sheep. Just take the combo. Stop complaining. Pay up. It’s your fault you don’t know how to read a formulary. #AmericaLosesAgain