Asthma Control: How to Use Inhalers Right, Avoid Triggers, and Manage Symptoms Long-Term

Most people with asthma think they’re doing fine as long as they don’t feel wheezy. But asthma isn’t just about symptoms-it’s about control. And right now, the rules have changed. If you’re still using a blue inhaler (SABA) alone, you’re not just outdated-you’re at higher risk for a life-threatening attack. New guidelines from 2025 make it clear: asthma control means using inhaled corticosteroids (ICS) every time you need relief, not just for daily prevention. This isn’t a suggestion. It’s the standard.
Why Your Blue Inhaler Alone Isn’t Enough
For decades, the go-to move for asthma was the blue rescue inhaler-albuterol, salbutamol, whatever brand you had. It worked fast. You felt better. So you kept using it. But here’s what no one told you: using it alone means your airways are still inflaming, silently, between attacks. The 2024 GINA update flipped the script. Now, every adult and teen with asthma, even if they only have symptoms once a month, should be on an ICS-containing medication. That means your rescue inhaler must contain corticosteroids, not just a bronchodilator.The VA/DOD 2025 guidelines put it bluntly: SABA-only treatment increases the chance of severe flare-ups and death. ICS-containing therapy, even when used only as-needed with a fast-acting LABA like formoterol, cuts that risk in half. In military populations, SABA-only prescriptions dropped from 57% of new cases in 2019 to just 22% by 2024. That’s not a coincidence. That’s science.
How to Use Your Inhaler Correctly (And Why It Matters)
You could have the best medication in the world, but if you’re not using your inhaler right, less than 20% of the drug actually reaches your lungs. Most people mess up in one of three ways:- They don’t shake the inhaler before use (for metered-dose inhalers)
- They press the canister and breathe in too slowly (dry powder inhalers need a fast, deep breath)
- They don’t hold their breath for 5-10 seconds after inhaling
The VA/DOD guidelines say: check inhaler technique at every visit. Not once a year. Every time. And they’re not just being picky. A study showed that patients who used their inhalers correctly had 40% fewer emergency visits over 12 months. If you’re unsure, ask your doctor for a spacer or a technique checklist. Some clinics even have video guides you can watch on your phone right in the exam room.
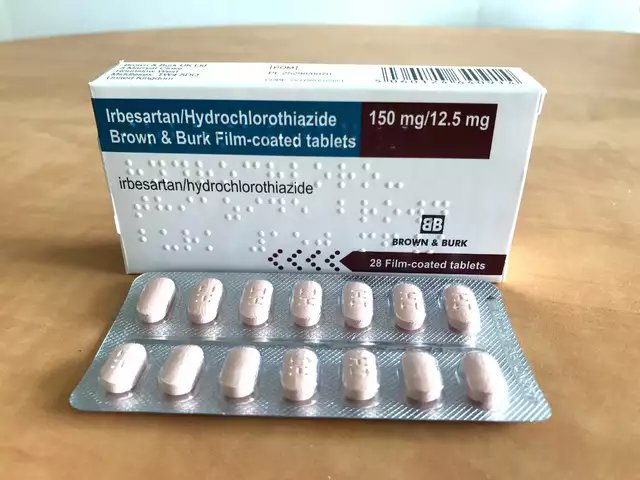
What’s in Your Inhaler? ICS, LABA, LAMA-What Do They Mean?
You don’t need to memorize medical jargon, but you do need to know what’s in your device:- ICS (Inhaled Corticosteroid): Reduces swelling and mucus in your airways. This is the core of modern asthma control. Dosing? Low: 50-250 mcg twice daily. Medium: 251-500 mcg. High: over 500 mcg. Higher mcg per puff means fewer puffs-easier to stick with.
- LABA (Long-Acting Beta-Agonist): Opens airways for 12+ hours. Always paired with ICS. Never used alone.
- LAMA (Long-Acting Muscarinic Antagonist): Added if you’re still struggling on ICS+LABA. Dose: 18 mcg once daily. Works differently than LABA, so it helps when the other two aren’t enough.
For most people with uncontrolled asthma, the new standard is a single inhaler that combines ICS and formoterol (a rapid-onset LABA). You use it as your daily controller AND your rescue inhaler. No more two inhalers. No more confusion. Just one device, used whenever you need it.
Triggers You Can’t Ignore (Even If You Think You Can)
Asthma isn’t just about what’s in your lungs-it’s about what’s around you. The NHLBI says: figure out your triggers. Not guess. Test. Skin or blood tests can show if you’re allergic to dust mites, pet dander, or mold. And if you’re not sure? Look for patterns. Do you cough more after laundry day? After a cold? After walking outside on a smoggy day?Common triggers include:
- Smoke (cigarettes, fireplaces, vaping)
- Pollen and mold (especially in spring and fall)
- Strong smells (perfume, cleaning sprays, paint)
- Exercise (but don’t skip it-use your inhaler 15 minutes before)
- Cold air (common in Calgary winters)
- Stress and strong emotions
- GERD (acid reflux-yes, stomach acid can trigger asthma)
- Obesity
One study found that people who reduced exposure to indoor allergens cut their rescue inhaler use by 60%. You don’t need to move out of your house. Start simple: wash bedding weekly in hot water, use HEPA filters, keep pets out of the bedroom, and seal gaps where mold can grow. If you smoke, quitting is the single most effective thing you can do for your lungs.
Long-Term Management: It’s Not Just Medication
Asthma control isn’t a checklist. It’s a lifestyle. The 2025 guidelines stress three pillars: medication, triggers, and education. That last one? It’s the one most people skip.Every person with asthma should have a written Asthma Action Plan. Not a generic printout. One made with your doctor. It should say:
- Which meds to take daily
- When to increase your dose
- When to call your doctor
- When to go to the ER
Use the Asthma Control Test (ACT) every 4-6 weeks. It’s five simple questions:
- Has your asthma kept you from doing normal activities?
- Have you had shortness of breath?
- Have you woken up at night because of asthma?
- Have you used your rescue inhaler more than twice a week?
- How would you rate your asthma control overall?
Score below 20? Your asthma isn’t controlled. Time to talk to your provider. Don’t wait until you’re in the ER.
Stepping Down: When and How to Reduce Medication
If your asthma has been stable for three months-no symptoms, no rescue use, no missed work or school-you might be able to reduce your meds. But don’t stop them. Ever.Guidelines say: reduce ICS by 25-50%. Don’t jump straight to zero. You can consider stopping LABA if you’re stable, but ICS stays. Why? Because inflammation doesn’t vanish just because symptoms do. Stopping ICS too soon is the #1 reason asthma comes back worse.
And if you’re on biologics? Those are for severe asthma. If your blood eosinophils are above 300 cells/μL or your FeNO (exhaled nitric oxide) is over 50 ppb, your doctor might recommend a targeted injection every few weeks. It’s not for everyone-but if you’ve tried everything else and still struggle, it’s worth discussing.
What’s New in 2025? The Big Shift
The biggest change? No more SABA-only treatment. Ever. That’s the rule now, from Canada to the U.S. to Europe. The NENC guidelines in the UK call it “Moving towards SABA-free asthma care.” The VA/DOD guidelines say the same. GINA calls it a “paradigm shift.”What does this mean for you?
- If you’re on a blue inhaler alone-ask your doctor for an ICS-containing option.
- If you have two inhalers (one blue, one brown)-you may be able to switch to one combo inhaler.
- If you’re using your rescue inhaler more than twice a week-your controller isn’t working. Time for a tune-up.
And yes, this applies to exercise-induced asthma too. You can still use a rescue inhaler before working out-but only if you’re also on daily controller therapy. No exceptions.
What Doesn’t Work (And Why)
There’s a lot of noise out there. Supplements, essential oils, breathing exercises, air purifiers. Some help. Most don’t change the disease.The NHLBI says: there’s no strong evidence that digital apps, smart inhalers, or wearable trackers improve outcomes beyond standard care. That doesn’t mean they’re bad-but don’t rely on them. Your inhaler technique, your trigger avoidance, and your ICS use? Those are what matter.
And no, you can’t out-exercise asthma. You can’t out-diet it. You can’t out-supplement it. Asthma is a chronic inflammatory condition. It needs targeted, consistent medical treatment.
Final Thought: Control Isn’t Perfect. But It’s Possible.
You don’t have to be symptom-free to have good asthma control. You just need to not be limited by it. No more skipping workouts. No more waking up gasping. No more panic when the weather changes. That’s the goal.And it’s not just possible-it’s standard. The science is clear. The tools are here. The only thing left is for you to use them right.





Herman Rousseau
December 22, 2025 AT 05:06Just switched to my new ICS/formoterol combo last month and wow. No more midnight coughing fits. No more panic before workouts. I used to rely on my blue inhaler like a crutch-now I use it maybe once a week. Game changer. 🙌
Vikrant Sura
December 22, 2025 AT 16:55Yeah right. Another corporate guideline pushed by Big Pharma. SABA works fine for me. Why pay more for fancy inhalers when the old one gets the job done? 🤷♂️
Candy Cotton
December 23, 2025 AT 23:33As an American citizen with a medical degree, I find it appalling that anyone would still be using SABA-only therapy. This is not a debate. It is a public health failure. The VA/DOD guidelines are clear, scientifically rigorous, and reflect the highest standard of care. If you’re not following them, you’re endangering yourself and others. Period.
Jeremy Hendriks
December 24, 2025 AT 08:02What is control anyway? Is it the absence of symptoms or the surrender to pharmaceutical inevitability? We treat asthma like a glitch in the system to be patched, not a conversation between body and environment. The inhaler is a bandage on a wound that refuses to name its cause. Maybe the real question isn’t how to use the device-but why we keep needing it in the first place.
Ajay Brahmandam
December 25, 2025 AT 08:16Been using the combo inhaler for 6 months now and honestly? Life’s easier. No more juggling two devices. Also, shaking the inhaler before use? I used to forget that too. Now I do it like a ritual before I leave the house. Small things matter. 😊
jenny guachamboza
December 27, 2025 AT 01:23Wait… so you’re telling me the government and pharma are forcing us to use expensive inhalers because they don’t want us to breathe naturally? 🤔 I read on a forum that air pollution from 5G towers is what’s really causing asthma… and they’re hiding the truth. Also, my cat is a government spy. 🐱👁️
Nader Bsyouni
December 28, 2025 AT 04:54Control is a construct. The inhaler is a tool of compliance. The real enemy is the illusion of management. You don’t tame asthma you negotiate with it. And if you think a pill in a canister can fix what modern life broke you’re missing the point entirely
Julie Chavassieux
December 28, 2025 AT 21:01...I just... I didn’t know... I thought I was fine... I’ve been using my blue inhaler every day for years... I didn’t realize... I’m so sorry... I didn’t know... I’m going to call my doctor tomorrow... I promise... I’m scared now...
Tarun Sharma
December 30, 2025 AT 11:14Good summary. Inhaler technique is often overlooked. I recommend practicing in front of a mirror. Many patients underestimate the importance of breath-hold. Small adjustments yield large results.
Gabriella da Silva Mendes
December 31, 2025 AT 11:21Okay but have you considered that maybe asthma isn’t even real? Like, maybe it’s just anxiety masquerading as lung trouble? I mean, I had this friend who got diagnosed and then she started using the inhaler and suddenly she could do yoga and drink kombucha and now she’s basically a wellness influencer. I think the whole thing is a scam. Also, my neighbor says the air in California is full of nanobots. So… yeah.
Kiranjit Kaur
January 2, 2026 AT 06:16My mom has asthma and she switched to the combo inhaler after her ER visit last year. She says she feels like she can finally breathe without thinking about it. That’s the goal, right? Not perfect, just peaceful. ❤️
Kathryn Weymouth
January 3, 2026 AT 13:49Thank you for emphasizing the Asthma Control Test. I’ve been using it monthly since my diagnosis and it’s the only objective metric I trust. My score went from 14 to 23 in six months. I didn’t realize how much I’d normalized suffering until I started measuring it.
Jim Brown
January 4, 2026 AT 08:54The inhaler is not merely a device-it is a covenant between the self and the body. To use it without understanding its purpose is to perform a ritual without meaning. The ICS is not a drug to suppress, but a signal to restore. We do not conquer asthma; we learn its language. And in that quiet dialogue, we find not control, but harmony.
Sai Keerthan Reddy Proddatoori
January 6, 2026 AT 03:55Why do Americans always think their way is best? In India we use nebulizers and home remedies. We don’t need fancy pills from big pharma. Also, the government is lying about everything. Why do you think they changed the guidelines? To sell more inhalers. I don’t trust it.