Post-Thrombotic Syndrome — August 2023 Archive
This month we covered Post-Thrombotic Syndrome (PTS), the common follow-up problem after a Deep Vein Thrombosis (DVT). If you had a DVT, PTS can show up months or even years later with pain, swelling, and skin changes in the affected leg. Our post explains what to watch for, what you can do at home, and when to see a doctor.
What PTS Looks Like
Pain and aching in the leg that gets worse when you stand or walk are typical. Swelling that won't go down after rest is a red flag. You may notice skin discoloration, tightness, or even ulcers in severe cases. Symptoms usually affect the same leg that had the DVT. They can be mild and annoying or serious enough to limit daily life.
PTS happens because the veins or their valves were damaged by the clot. That damage makes it harder for blood to flow back to the heart, so fluid builds up in the leg. The risk of PTS is higher when the DVT was large, untreated, or in the thigh or pelvis.
Practical Prevention and Care Tips
Want to lower your chances of getting PTS? Follow these practical steps. First, stick to your anticoagulant plan exactly as prescribed. Stopping early increases the risk of more clots and more vein damage. Second, wear proper compression stockings if your doctor recommends them. They help reduce swelling and improve vein flow. Third, keep moving. Gentle walking and calf exercises help the muscle pump that pushes blood up the leg.
At home, elevate your leg when you can. Avoid long periods of standing or sitting without breaks. Maintain a healthy weight and quit smoking — both help vein health. If you travel, get up and walk every hour on long trips. When you stand or sit, flex your ankles and toes to keep blood moving.
If you already have symptoms, start basic care right away. Use compression stockings daily if they help. Apply simple pain relief like over-the-counter painkillers if needed and approved by your doctor. Keep an eye on your skin. Treat any breaks or sores promptly and seek medical care for wounds that don’t heal.
Some people need more than home care. Doctors can offer procedures to remove clots, open blocked veins, or place stents in selected cases. Referral to a vascular specialist is common when symptoms are severe or progressive. Physical therapy can also help by teaching exercises and compression techniques that ease symptoms.
When should you see the doctor? If pain or swelling is sudden or severe, get immediate care — that could signal a new clot. If swelling gradually worsens, or skin changes or ulcers appear, make an appointment. Regular follow-up after a DVT helps catch PTS early and keeps treatment options open.
August 2023 focused on clear, usable guidance: know the signs, stick to treatment, use compression, move more, and get specialist help when needed. If you’ve had a DVT, watch your legs and act early — small steps now can prevent bigger problems later.
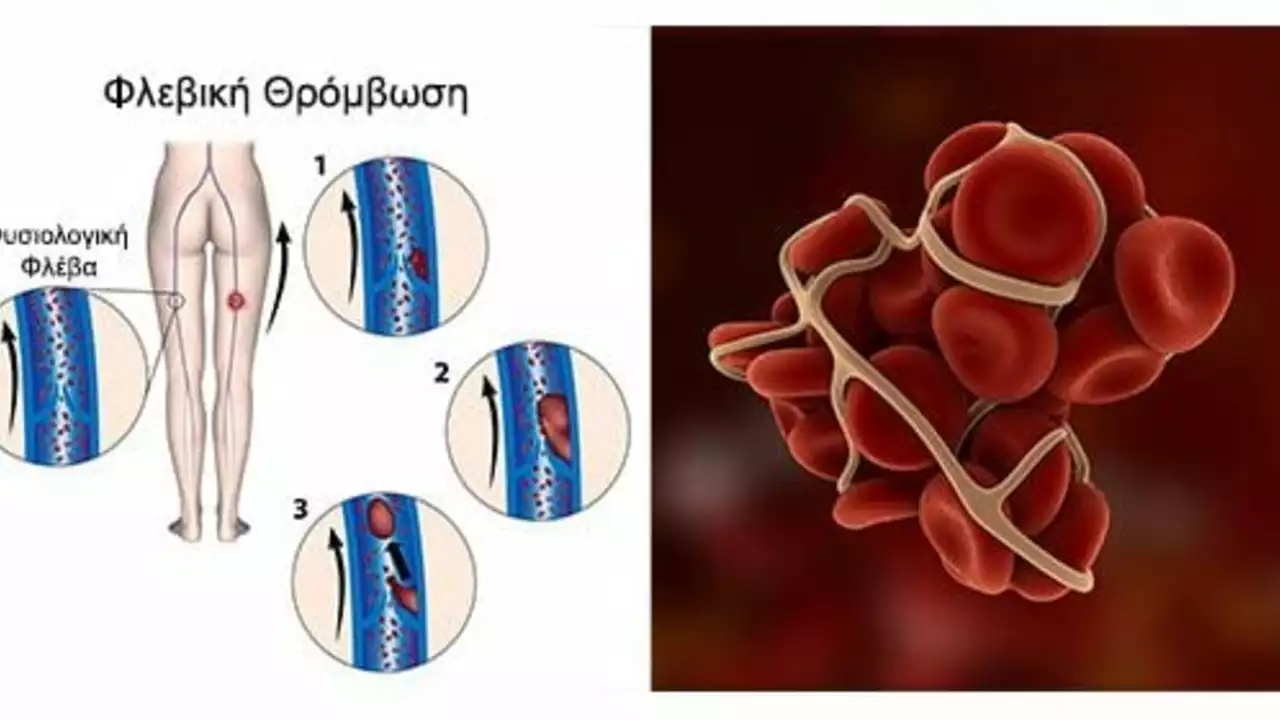
Post-Thrombotic Syndrome: A Common Complication of Deep Vein Thrombosis
Well, folks, here we go! Post-Thrombotic Syndrome, or as I like to call it, "the annoying aftermath of Deep Vein Thrombosis." It's like that one guest who just doesn't know when to leave the party. Essentially, it's a common complication that may follow a bout of Deep Vein Thrombosis (DVT). It's a tricky little number, causing symptoms like pain, swelling, and skin changes in the affected limb. So, if you've had DVT, keep an eye out for this persistent party crasher!
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)