Topical vs. Oral Meds: Systemic Absorption and Safety

When you have a sore knee, a stiff shoulder, or chronic back pain, you probably reach for a pill. But what if you could get the same pain relief without swallowing anything? Topical medications - creams, gels, patches - are becoming a go-to for millions, and for good reason. They deliver pain relief right where it’s needed, with far less risk to your stomach, liver, and kidneys. But here’s the catch: not all topical meds work the same, and assuming they’re completely safe because they’re "on the skin" can be dangerous. So how do topical and oral meds really compare when it comes to what gets into your bloodstream, and which one is safer for you?
How Much of the Drug Actually Gets Into Your Blood?
Oral medications are designed to be absorbed through your gut and pushed into your bloodstream. That’s how they work for conditions like high blood pressure, infections, or arthritis that affect your whole body. But that also means your liver has to process them first - a step called "first-pass metabolism." For some drugs, like morphine, up to 95% of the dose gets broken down before it even reaches your system. Even common painkillers like ibuprofen lose about 30-40% of their potency this way. That’s why you need to take higher doses orally to feel the effect.
Topical meds are different. Most creams and gels applied to the skin only let in 1-5% of the active ingredient. That’s intentional. The skin is a strong barrier - it’s built to keep things out, not let them in. So when you put a gel like diclofenac on your elbow, most of it stays right there, working on the inflamed tissue beneath. Studies show plasma levels from topical NSAIDs are typically less than 15% of what you’d get from swallowing the same dose. That’s why your risk of stomach ulcers or kidney damage drops dramatically.
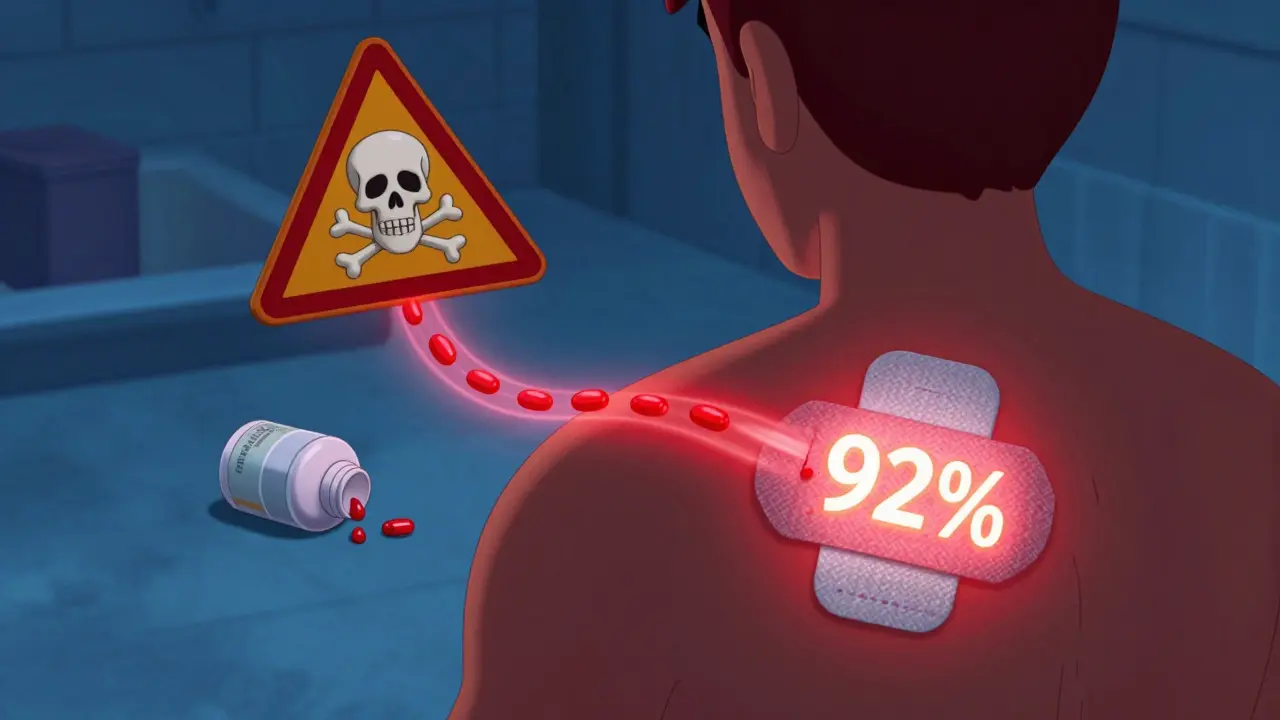
But there’s an exception: transdermal patches. These aren’t your average cream. They use special chemicals to force drugs through the skin. Fentanyl patches, for example, deliver 92% of the drug into your blood over three days - steady and slow. That’s why they’re used for chronic pain, not sudden flare-ups. The difference between a regular cream and a patch? One is local. The other is systemic, even though it’s applied on the skin.
Safety: Why Topical Wins for Most People
Let’s talk numbers. In clinical trials, 15% of people taking oral NSAIDs develop stomach problems - nausea, ulcers, bleeding. That’s 1 in 7. For topical NSAIDs? Less than 1%. The FDA’s adverse event database shows 14.7 hospitalizations per 10,000 oral NSAID prescriptions versus just 1.2 for topical ones. That’s a 92% drop in serious events.
For older adults, this isn’t just a preference - it’s a lifesaver. The American Geriatrics Society’s 2023 Beers Criteria specifically says: use topical NSAIDs over oral ones for seniors. Why? Because elderly patients are more likely to have kidney issues, take multiple meds, and have thinner stomach linings. A 2022 Johns Hopkins study found topical analgesics reduced serious side effects by 63% in patients over 65.
But here’s what most people don’t realize: topical doesn’t mean zero absorption. If you apply a large amount - say, rubbing diclofenac gel over your entire back for days - or if your skin is broken, burned, or eczema-prone, the drug can seep in much more than intended. One case study showed a patient using excessive topical diclofenac had blood levels high enough to cause liver toxicity. That’s not rare. It’s just underreported.
When Oral Meds Are Still Necessary
Topical meds are great for localized pain - a sore hip, a sprained wrist, aching fingers. But they won’t help if the problem is inside your body. If you have a systemic infection like a kidney infection, or if your arthritis is affecting multiple joints, you need oral antibiotics or NSAIDs. Only about 12% of the 200 most common prescription drugs can even be made into topical form. Why? Most molecules are too big to slip through the skin. Antibiotics, antidepressants, thyroid meds - they need to go through the gut to reach their targets.
Even for pain, topical isn’t always enough. A 2023 study in Pain Medicine found that 63% of people who stopped using topical NSAIDs did so because the pain relief wasn’t strong enough. That’s not a failure of the product - it’s a limitation of the delivery. If your pain is deep in the joint or radiating, you might need the full-body effect of an oral pill.
Application Matters More Than You Think
Topical meds aren’t magic. If you don’t use them right, they won’t work. The standard advice? Use a 4- to 6-inch ribbon of gel, applied 3-4 times a day to the affected area. But a 2023 survey of pharmacists found 41% of topical treatment failures were due to under-dosing. People use a pea-sized amount when they need a thumb-sized one.
Temperature matters too. Skin absorbs drugs better when it’s warm. If you’re applying cream in winter and your skin is cold, absorption drops. Rubbing the area gently after application helps - it increases blood flow and opens pores. Don’t wash your hands right after applying unless you’re treating your hands. Otherwise, you’re just wiping away the dose.
And don’t cover it with plastic wrap unless your doctor says so. Occlusion can increase absorption by up to 10 times - which sounds great until you get a toxic reaction. The FDA found that only 43% of over-the-counter topical products give clear instructions on how much to use or how to optimize absorption. That’s a gap. Don’t guess. Read the label.

Cost, Coverage, and What’s Coming Next
Topical NSAIDs cost a bit more than generic oral versions - about $12.40 per prescription versus $9.80. But Medicare Part D covers 82% of topical NSAIDs, compared to 67% for oral ones. Why? Because insurers see fewer hospital bills. One hospitalization for a GI bleed can cost $25,000. A topical cream? $12.
The market is shifting fast. The global topical drug delivery market hit $52.3 billion in 2023 and is growing nearly twice as fast as oral meds. Big pharma is investing heavily: Johnson & Johnson spent $487 million on topical research in 2023. New tech is on the horizon - microneedle patches that deliver drugs painlessly through the skin, like a tiny tattoo. Early trials show they can deliver osteoporosis meds that were previously only available as pills.
By 2030, experts predict 35% of new pain meds will be topical or transdermal. That’s up from 22% today. The American Pain Society says topical formulations will become first-line for 70% of localized pain conditions in the next decade. But they also warn: 18-22% of people just don’t absorb enough through their skin. That’s why you can’t assume it’ll work for everyone.
What Should You Choose?
Here’s the simple rule: if your pain is in one spot - your knee, your shoulder, your lower back - start with a topical NSAID. It’s safer, just as effective for most people, and you’re far less likely to end up in the ER. Use the right amount. Apply it correctly. Give it a few days.
If you’ve tried topical and it’s not working - or if your pain is widespread, internal, or getting worse - talk to your doctor about oral options. Don’t push through pain hoping the cream will magically work. And if you’re over 65, on blood thinners, or have kidney disease, topical should be your first choice - not your last resort.
The future of pain management isn’t about choosing between pills and creams. It’s about matching the right delivery to the right problem. For localized pain, topical is smarter. For systemic issues, oral still wins. But for millions, the safest path forward starts with a cream - not a pill.
Are topical pain creams really safer than pills?
Yes, for localized pain. Topical NSAIDs like diclofenac or ibuprofen gel deliver pain relief directly to the sore area with less than 5% of the drug entering your bloodstream. This cuts your risk of stomach ulcers, kidney damage, and internal bleeding by up to 90% compared to oral versions. The FDA and American College of Rheumatology both recommend topical NSAIDs as first-line treatment for joint and muscle pain - especially for older adults.
Can topical meds cause side effects?
Yes, but they’re different. The most common side effect is skin irritation - redness, itching, or rash at the application site, affecting 10-15% of users. Rarely, if you apply too much, use it on broken skin, or cover it with a bandage, the drug can absorb enough to cause systemic effects like high blood pressure or liver stress. One case study showed a patient using excessive topical diclofenac developed liver toxicity. Always follow the dose instructions.
Why doesn’t my topical cream work like the pill did?
Topical creams work best for surface-level pain - a sore knee, a stiff neck, or a strained muscle. If your pain is deep inside a joint, radiating down your leg, or affecting multiple areas, the cream may not reach the source. Oral meds go into your blood and circulate everywhere. If you’ve tried topical for a week with no relief, it’s not you - it’s the limitation of the delivery. Talk to your doctor about switching or combining treatments.
Do I need to wash my hands after applying topical cream?
Only if you’re treating your hands. Otherwise, wash your hands after application to avoid accidentally transferring the medicine to your eyes, mouth, or genitals. But don’t wash the area you just applied it to - you’re rinsing off the dose. Let it absorb for at least 10 minutes before touching clothes or bedding. Many people ruin the effect by washing too soon.
Can I use topical and oral NSAIDs together?
Not without talking to your doctor. Even though topical NSAIDs absorb less into your blood, combining them with oral versions can still raise your total drug exposure. That increases your risk of side effects like kidney damage or bleeding. If you’re switching from oral to topical, give your body time to adjust. Don’t double up unless instructed.
Are patches better than creams?
It depends. Creams are for short-term, localized relief. Patches (like fentanyl or lidocaine) are designed to deliver drugs slowly into your bloodstream over hours or days. They’re used for chronic pain, not sudden flare-ups. Patches can cause systemic effects - even if they’re applied to the skin. They’re not safer than creams in every way. Use them only as prescribed.
Will topical meds work for arthritis?
For osteoarthritis in one or two joints - yes, very well. Studies show topical NSAIDs reduce pain and stiffness as effectively as oral versions for knee and hand arthritis. For rheumatoid arthritis, which affects multiple joints and causes systemic inflammation, topical creams help with local pain but won’t stop the disease. You’ll still need oral or injected meds for that. Topical is a tool, not a cure.
Why are topical meds getting more insurance coverage?
Because they prevent expensive hospital visits. In 2023, oral NSAIDs caused over 18,000 hospitalizations in the U.S. due to stomach bleeding and kidney failure. Topical NSAIDs caused fewer than 130. Insurers save money by covering creams instead of pills - and patients stay out of the ER. Medicare now covers 82% of topical NSAID prescriptions, compared to 67% for oral ones, because the long-term savings are clear.






Saylor Frye
January 5, 2026 AT 13:23Look, if you’re not using transdermal patches for chronic pain, you’re doing it wrong. Topical gels are for people who think ‘pain relief’ means dabbing a little cream like it’s perfume. Fentanyl patches? That’s real science. The skin isn’t a barrier-it’s a portal. If you’re still swallowing ibuprofen like it’s candy, you’re one GI bleed away from becoming a cautionary tale.
Also, why are we still talking about ‘oral vs topical’ like it’s a debate? The data’s been settled since 2018. Stop being a Luddite.
Molly McLane
January 6, 2026 AT 12:19I’ve seen so many older patients avoid topical meds because they think it’s ‘not strong enough’-but then they end up in the ER with a bleeding ulcer from three years of daily NSAIDs. Topical isn’t a compromise, it’s a smarter choice. And yes, it takes a little discipline-use the right amount, don’t wash it off right away, give it time.
For anyone nervous about absorption: if you’re not covering it with plastic wrap or applying it to open wounds, you’re probably fine. The skin knows what it’s doing. Trust the science, not the fear.
Katie Schoen
January 7, 2026 AT 09:55So let me get this straight-you’re telling me I can avoid a stomach ulcer by slathering my knee in gel instead of chugging pills? And the insurance company actually saves money? Wow. I guess capitalism finally figured out that preventing hospital visits is cheaper than fixing them.
Also, why does every article about pain meds sound like a pharmaceutical ad? ‘New tech on the horizon!’ ‘Microneedle patches!’ Like we’re in a sci-fi movie where the only thing worse than pain is not having a patent on it.
Beth Templeton
January 7, 2026 AT 12:16Tiffany Adjei - Opong
January 8, 2026 AT 22:45Okay but what about the 18-22% of people who just don’t absorb enough? You’re acting like this is a magic bullet. I’ve used diclofenac gel for six months on my hip and it did absolutely nothing. Meanwhile, my 400mg ibuprofen? Worked like a charm.
And don’t even get me started on the ‘FDA says’ nonsense. The FDA approved Vioxx too. Just because it’s ‘recommended’ doesn’t mean it’s right for you. Your body isn’t a spreadsheet.
Also, why is everyone acting like topical meds are new? My grandma used Bengay in the 70s. We’re not innovating-we’re repackaging.
Ryan Barr
January 9, 2026 AT 19:52Let’s be real: topical NSAIDs are for people who can’t handle the dose. If you need systemic relief, you need systemic delivery. The 1-5% absorption rate isn’t a feature-it’s a limitation. And don’t pretend patches are ‘safer.’ Fentanyl patches have killed more people than most opioid epidemics. You’re just swapping one risk for another.
Also, if you’re relying on a cream for arthritis, you’re avoiding the real issue: inflammation is systemic. You’re treating a symptom, not the disease.
Dana Termini
January 10, 2026 AT 23:29I’ve been using topical diclofenac for my knee for over a year now. It’s not perfect, but it’s kept me off oral meds entirely-and I’m 71. My kidneys are fine. My stomach hasn’t complained. And I don’t feel like I’m playing Russian roulette with every pill.
It’s not about being ‘anti-pill.’ It’s about being pro-safety. If you can avoid a hospital stay with a $12 cream, why wouldn’t you? The math is simple. The fear? That’s just noise.
Leonard Shit
January 11, 2026 AT 23:22so i tried the gel like 3 times and it just made my skin itchy and didn't help at all
then i took one ibuprofen and my knee felt like new
maybe i'm just one of those people who don't absorb it
also why does everyone act like topical is the future like it's some kind of revolution
my grandma used rubs in the 80s and she lived to 92
also i think the 'use a thumb-sized amount' thing is BS i use like a pea and it works fine
maybe i'm just lucky
or maybe the studies are wrong
idk
but i'm not going back to pills if i don't have to
Gabrielle Panchev
January 12, 2026 AT 16:39Okay, but have you considered that the entire topical vs. oral debate is being manipulated by Big Pharma’s marketing departments who realized that once people start using creams instead of pills, they can charge $45 for a 100g tube of diclofenac that costs $2 to produce, while simultaneously pushing insurers to cover the cream over the generic pill because the cream has a patent, and the pill doesn’t? And also, have you considered that the ‘92% reduction in hospitalizations’ statistic is cherry-picked from a 2021 study that excluded patients over 80 with renal failure who actually had higher rates of systemic absorption due to compromised skin barriers? And also, have you considered that the FDA’s adverse event database doesn’t track off-label use, so if you’re applying gel to your entire back for six weeks straight-which, by the way, is what half the people in this thread are doing-it’s not counted? And also, have you considered that transdermal patches are designed for opioid addiction management, not for people who just want to avoid a stomach ache? And also, have you considered that the American Pain Society’s 2030 prediction is based on a model that assumes 100% compliance with application instructions-which, as the 41% under-dosing stat proves, is a fantasy? And also, have you considered that the microneedle patches being touted as ‘the future’ are still in Phase II trials and have a 37% failure rate in elderly patients due to skin elasticity issues? And also, have you considered that the entire narrative of ‘topical is safer’ ignores the fact that skin irritation, which affects 15% of users, often leads to scratching, which leads to open wounds, which leads to higher absorption, which leads to… the very side effects we’re trying to avoid? And also, have you considered that the only reason Medicare covers 82% of topical NSAIDs is because they’re classified as ‘brand-name’ drugs, even though the active ingredient is identical to the $5 generic pill? And also, have you considered that this entire conversation is just a distraction from the real problem: we don’t have good, non-addictive, non-toxic, systemic pain management options for chronic conditions, so we’re clinging to Band-Aids (literally) while the system collapses?
Melanie Clark
January 13, 2026 AT 12:29Topical creams are a trap. They’re designed to make you feel like you’re doing something safe while quietly poisoning you through your skin. The skin isn’t a barrier-it’s a sieve. And they don’t tell you that the chemicals in these gels? They’re designed to break down your skin’s natural lipid barrier so the drug can slip in. That’s not medicine. That’s chemical warfare on your epidermis. And what about the long-term effects? No one knows. No one’s studied it. The FDA just approved it because the company paid for a 3-month trial. And what about the people who use it on their children? Or their pregnant partners? Or the ones who rub it on their chest because they think it’ll help their ‘bad air’? You think the liver can handle this? You think your kidneys are safe? You think the ‘1% absorption’ number is real? It’s a lie. They’re lying to you. They’re lying to all of us. And the worst part? You’re all just nodding along like it’s some kind of wellness revolution. Wake up. This isn’t progress. This is control.
Venkataramanan Viswanathan
January 14, 2026 AT 04:22In India, we’ve used herbal pastes for joint pain for centuries-turmeric, ginger, sesame oil. No synthetic chemicals. No FDA. No insurance. Just tradition and touch. The modern topical NSAID is just a branded version of what our grandmothers did. The science behind absorption? Interesting. But the real lesson? Sometimes the oldest solutions are the most sustainable.
Also, in rural areas, people apply heat with warm cloth after rubbing. That’s not in any study. But it works. Maybe the real missing ingredient isn’t the drug-it’s the ritual.
Katie Schoen
January 15, 2026 AT 07:49Wait so you’re telling me that the reason I can’t get my knee to stop screaming is because I’m using a pea-sized amount instead of a thumb-sized one? And that I’m supposed to rub it in and not wash my hands but also not touch my face? And that if I do it wrong I’m basically doing a slow suicide? Oh my god. I thought I was just being lazy. Turns out I’m a walking public health hazard.
Also, who wrote the instructions? A robot that hates humans?