Societal Approaches to Health: What Actually Works
Public health isn’t just about medicines and hospitals — it’s about how communities, laws, and everyday people shape outcomes. You can see the impact in real life: communities with strong social support keep people healthier and help them recover faster. That’s not fluff — social ties change behavior, improve follow-up care, and lower stress, and those things affect blood pressure, diabetes control, and recovery after surgery.
Community-level actions that help
Start local. Neighborhood programs that pair volunteers with older adults for weekly check-ins cut isolation, catch medication issues early, and keep emergency room visits down. Community health workers who know local languages and customs make a big difference when they help people navigate prescriptions, insurance, or complex treatment plans. Practical moves like local drug take-back events, free screening days, and pop-up clinics bring care to people who can’t travel or take time off work.
Schools and workplaces matter too. Simple policies — paid sick leave, flexible hours for medical visits, and clear on-site referral paths — reduce delays in care. Employers who connect staff to reliable telehealth or price-transparency tools help people find affordable medications without risking health or finances.
Policy, NGOs, and reducing barriers
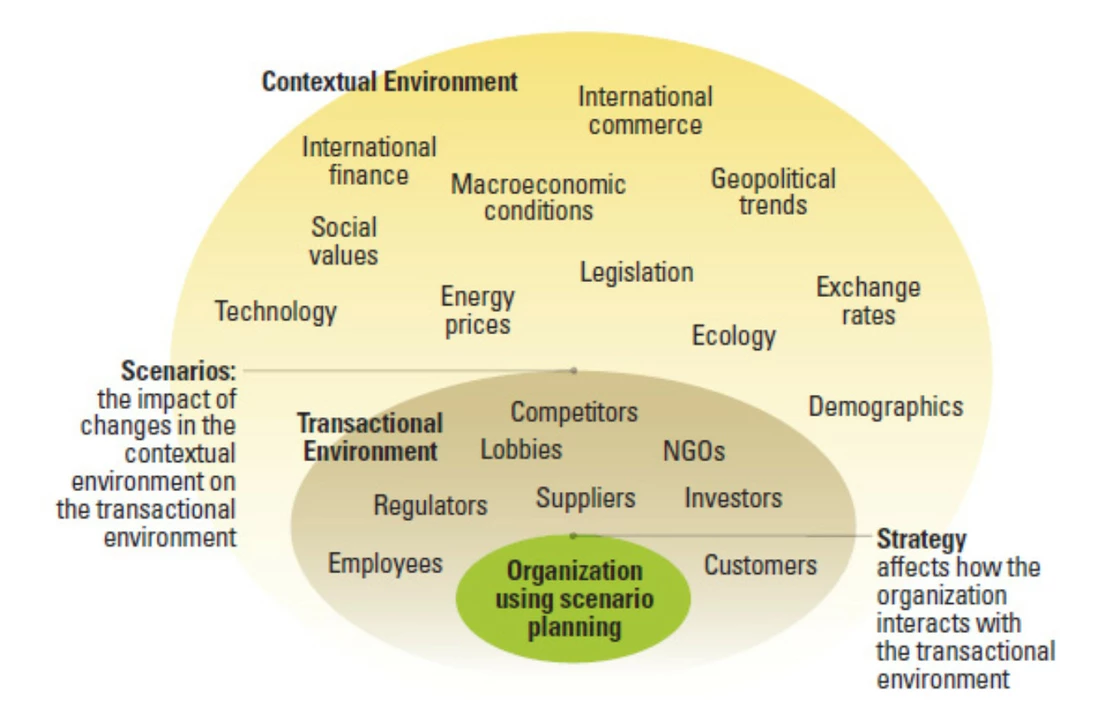
Policy changes shape access faster than individual efforts. Laws that require price transparency let people compare prescription costs and avoid hidden fees. Expanding coverage for preventive services and mental health lowers long-term spending and keeps people out of crisis care. NGOs and grassroots groups fill gaps where the system falls short — helping with transport to clinics, negotiating lower drug prices, or running family planning clinics. When NGOs work with public agencies, solutions scale up faster and reach underserved groups.
Stigma is a major barrier. For issues like mental health, HIV, or family planning for LGBT people, fear of judgment stops people from seeking help. Campaigns that normalize care, share real stories, and offer confidential services increase uptake. Practical step: local clinics can offer anonymous appointment options and staff training on respectful communication to make care feel safe.
Want to act now? Join or start a neighborhood health group, ask your clinic about patient navigation services, and support local policies for price transparency and paid sick leave. If you’re part of a nonprofit, partner with community leaders to tailor programs to real local needs instead of guessing what people want.
Small, smart societal changes add up. When communities, clinics, and policymakers work together, access improves, costs drop, and people get care that fits their lives. That’s a practical, powerful approach you can support today.
Bed-wetting and cultural differences: How various societies approach the issue
As a blogger, I've recently delved into the topic of bed-wetting and how different cultures approach this issue. It's fascinating to see how various societies around the world handle such a common problem. Some cultures view bed-wetting as a natural part of a child's development, while others may consider it a cause for concern or shame. In some cases, traditional remedies and practices are used to address the issue, while in others, modern medical interventions are sought. Overall, the approach to bed-wetting varies greatly across cultures, highlighting the importance of understanding and respecting these differences.
Categories
- Medications (70)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



