Prostate cancer: Signs, screening, and treatment
Prostate cancer is one of the most common cancers in men. You might not notice anything at first, and that’s exactly why knowing the signs and screening options matters. This page gives clear, practical steps for spotting issues early, understanding tests like the PSA, and weighing treatment choices without medical jargon.
Symptoms and when to see a doctor
Early prostate cancer often has no symptoms. When symptoms appear, they usually involve the urinary system: weak stream, needing to pee more at night, or trouble starting and stopping urination. Blood in urine or semen, pain during ejaculation, or persistent lower back and hip pain can also show up in advanced cases. If any of these occur, don’t ignore them—book an appointment. These signs can come from other, less serious conditions, but only a doctor can tell for sure.
Worried but feeling fine? Talk to your doctor about screening if you’re over 50, or over 45 with higher risk (family history or Black men). Screening is a personal choice: it can find cancer early but may also lead to extra tests you don’t need. Discuss pros and cons based on your health and life goals.
Diagnosis and treatment options
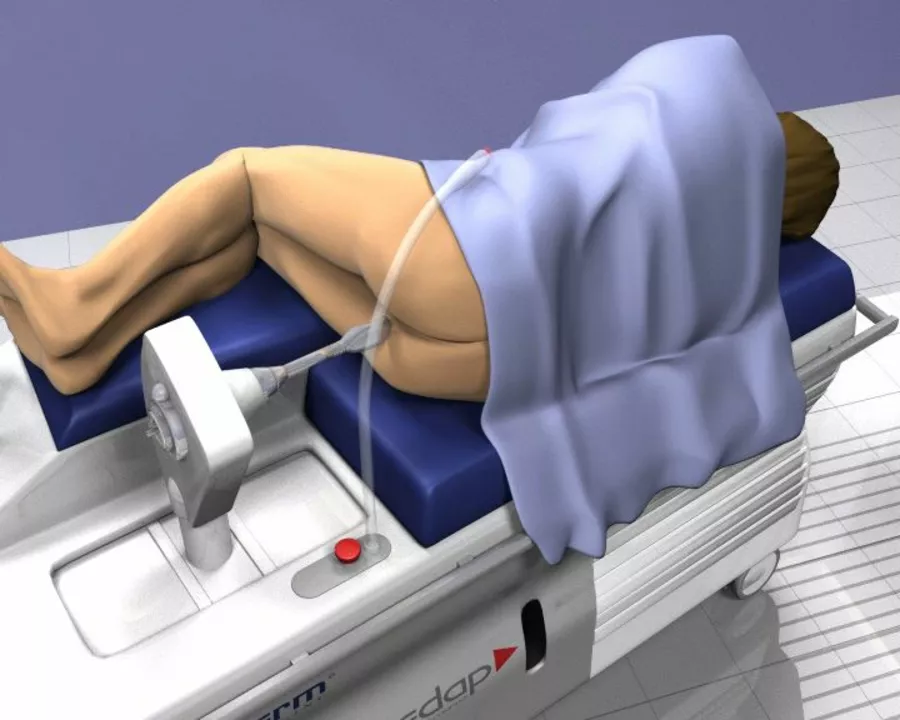
Diagnosis usually starts with a PSA blood test and a digital rectal exam (DRE). A high PSA or abnormal DRE may lead to a prostate biopsy and imaging like MRI. Pathology results tell if cancer is present and how aggressive it is. That info guides treatment choices.
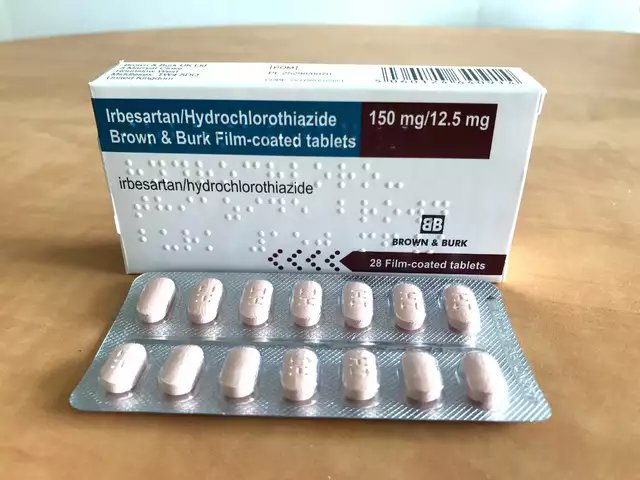
Treatment ranges from active surveillance to surgery, radiation, hormone therapy, and chemotherapy. Active surveillance means regular tests and scans for slow-growing cancers. Surgery (prostatectomy) removes the prostate and can cure early disease but may cause side effects like erectile dysfunction or urinary changes. Radiation treats the prostate from outside or inside and has a different side-effect profile. Hormone therapy lowers testosterone to slow cancer growth and is often used for more advanced disease. Chemotherapy is typically for cancers that no longer respond to hormone therapy.
Choosing a treatment depends on cancer stage, your age, other health issues, and your priorities. Want to keep sexual function or avoid surgery? Tell your team. Want the most aggressive option available? That’s valid too. A second opinion is helpful when choices feel big and confusing.
Simple lifestyle steps can help overall health during and after treatment: stay active, eat a balanced diet, quit smoking, and manage weight. These won’t cure prostate cancer, but they improve outcomes and quality of life.
Got questions or symptoms? Start by calling your primary care doctor or a urologist. Early conversations lead to smarter choices. If you have a family history, mention it—doctors might recommend earlier screening. Your health decisions should fit your life, not a one-size-fits-all rule.
Real-Life Stories: How Enzalutamide Has Helped Prostate Cancer Patients
I recently came across some incredible real-life stories of prostate cancer patients who have benefited from Enzalutamide, an advanced treatment option. These inspiring accounts showcase the significant improvement in patients' quality of life and the prolongation of survival rates. Many individuals shared their gratitude for this breakthrough medication, as it has allowed them to continue leading fulfilling lives. In my blog, I have highlighted these powerful stories to raise awareness and provide hope for those currently battling prostate cancer. Enzalutamide has truly made a positive impact in the lives of countless patients and their families.
Categories
- Medications (70)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)