Potassium levels: what they mean and what to do
Potassium is a mineral your muscles, nerves, and heart need to work. Blood potassium is measured in mmol/L. Most labs call 3.5–5.0 mmol/L normal. Below 3.5 is hypokalemia; above 5.0 is hyperkalemia. Small shifts can cause big symptoms, so paying attention matters.
What abnormal potassium looks and feels like
Low potassium (hypokalemia) often causes muscle cramps, weakness, constipation, and tiredness. If it gets severe you may notice palpitations or fainting. Common labs: mild 3.0–3.4 mmol/L, moderate 2.5–3.0, severe under 2.5.
High potassium (hyperkalemia) can give burning or tingling, muscle weakness, and dangerous heart rhythm changes. If potassium rises over about 6.0 mmol/L, the risk of sudden serious arrhythmias goes up. ECG changes to watch for are peaked T waves, flattened P waves, and a widened QRS complex.
What to do: tests, causes, and practical steps
Get a basic metabolic panel (BMP) or serum potassium if you have symptoms, take certain meds, or have kidney disease. If a single result is odd, doctors often repeat the test and check an ECG before acting.
Common causes of low potassium: loop or thiazide diuretics (furosemide, hydrochlorothiazide), vomiting, diarrhea, excessive sweating, and insulin shifts. Low potassium is treated with oral potassium chloride for mild cases; severe cases need IV potassium in the hospital with heart monitoring. Never give IV potassium at home.
Common causes of high potassium: reduced kidney function, ACE inhibitors or ARBs, potassium-sparing diuretics (spironolactone), NSAIDs, trimethoprim, and taking too much potassium or salt substitutes. For acute high potassium, emergency treatments in hospital include IV calcium (to stabilize the heart), insulin with glucose (to move potassium into cells), nebulized albuterol, and dialysis if needed. Newer outpatient drugs like patiromer bind potassium in the gut for chronic control.
Diet tips: if your potassium is low, eat potassium-rich foods like a medium banana (~400 mg), a medium baked potato (~900 mg), a cup of cooked spinach (~800 mg), or a cup of beans (~600 mg). If your potassium is high, limit those foods and check product labels and salt substitutes (many are potassium-based).
Medication check: tell your provider about all meds and supplements. Don’t start potassium tablets or high-dose supplements without a doctor’s okay. If you feel sudden chest pain, severe weakness, or fainting—go to the ER. For non-urgent changes (mild symptoms, routine results), call your healthcare team to plan repeat labs and safe adjustments.
Small steps — repeat tests, review meds, adjust diet — often fix mild problems. For anything severe, get immediate medical help. Your heart and muscles will thank you for acting early.
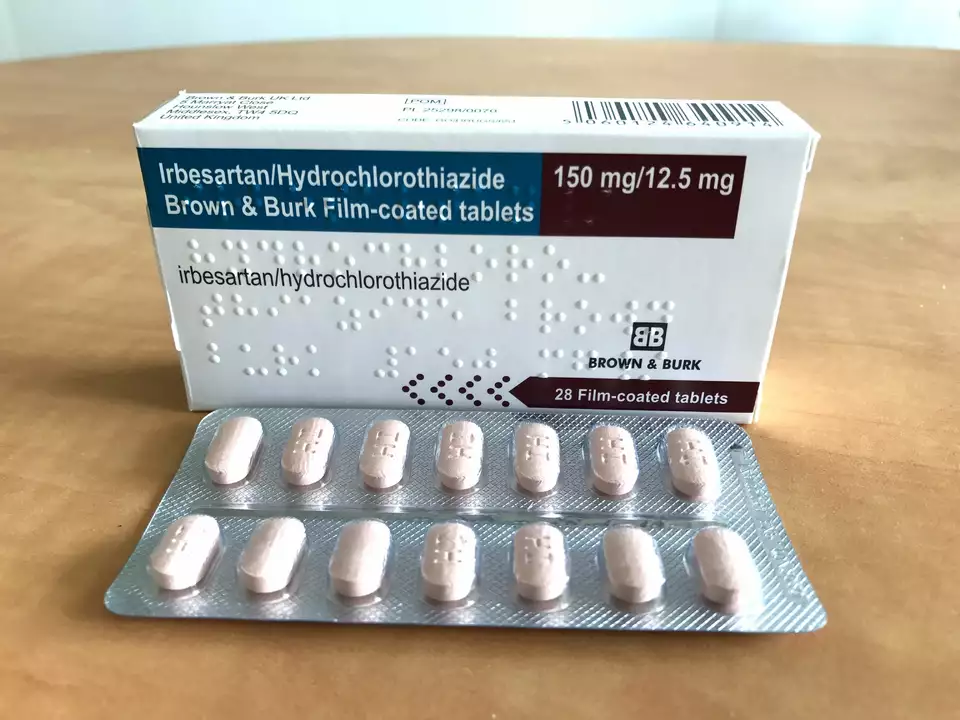
The Effects of Irbesartan Hydrochlorothiazide on Potassium Levels
I recently came across a study on the effects of Irbesartan Hydrochlorothiazide on potassium levels in the body. This medication is commonly used to treat high blood pressure and can significantly impact our potassium levels. The results showed that while some patients experienced a decrease in potassium, others maintained normal levels or even experienced an increase. It's important to monitor potassium levels when taking this medication, as imbalances can lead to health complications. Always consult your doctor for personalized advice and proper dosage adjustments.
Categories
- Medications (70)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)
Popular Articles



