Pituitary Tumor: What You Need to Know
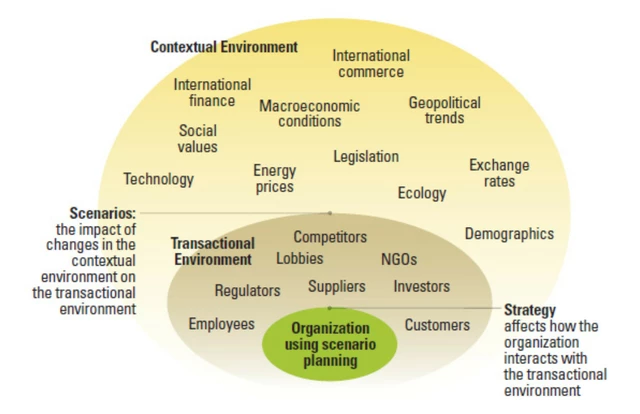
When dealing with pituitary tumor, an abnormal growth in the pituitary gland that can disrupt hormone production and press on nearby structures, it helps to start with the organ itself. The pituitary gland, a pea‑sized endocrine hub at the base of the brain that regulates growth, metabolism, and reproduction releases hormones that travel through the bloodstream to control almost every body system. When a growth becomes a adenoma, a usually benign tumor that makes up the majority of pituitary lesions, it may stay silent or cause a cascade of issues. A tumor encompasses structural change, influences hormone levels, and requires a multidisciplinary response. Patients often notice symptoms because a hormone‑secreting adenoma floods the body with excess prolactin, ACTH, or growth hormone, leading to irregular periods, unexplained weight gain, or enlarged hands and feet. Alternatively, a non‑functioning tumor can press on the optic chiasm, producing tunnel‑vision or blurry peripheral vision. The diagnostic pathway follows a clear logical chain: the tumor necessitates detailed imaging, blood work, and endocrine assessment to pinpoint its type and size.
Key Aspects: Imaging, Hormone Therapy, and Surgery
Accurate imaging is the backbone of pituitary tumor work‑up. A high‑resolution MRI scan, magnetic resonance imaging that visualizes the gland and surrounding brain tissue reveals the lesion’s dimensions, its relationship to the optic nerves, and whether it has invaded nearby structures. Blood tests then measure hormone panels—prolactin, cortisol, thyroid‑stimulating hormone, among others—to classify the tumor’s secretory behavior. Once the data are in hand, doctors can decide between medical and surgical routes. Hormone therapy, medications such as dopamine agonists for prolactin‑secreting tumors or somatostatin analogues for growth‑hormone excess often shrink the tumor and normalize hormone levels, sparing many patients from invasive procedures. When medication isn’t enough or the tumor threatens vision, pituitary surgery, typically a transsphenoidal approach done through the nasal cavity becomes the preferred option. Surgeons aim to remove as much of the adenoma as possible while preserving normal gland tissue, reducing the risk of postoperative hormone deficits. After surgery, patients may need temporary hormone replacement and regular MRI checks to catch any recurrence early. The whole care continuum—imaging, medical management, and surgery—forms a tightly linked loop that maximizes the chance of cure and quality of life.
Below you’ll find a curated list of articles that dive deeper into each of these steps, from how to interpret MRI results to choosing the right medication and what to expect after surgery. Whether you’re just hearing the term “pituitary tumor” for the first time or you’re managing a diagnosis, the posts ahead break down complex concepts into practical, easy‑to‑apply advice you can use right away.
Acromegaly and Pituitary Tumors: What’s the Connection?
Explore how pituitary tumors cause acromegaly, learn symptoms, diagnosis steps, treatment options, and long‑term management for better health.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)