Loteprednol Dosage: What You Need to Know
When working with loteprednol, a soft‑targeted corticosteroid used for eye and skin inflammation. Also known as Lotemax, it offers strong anti‑inflammatory effects while minimizing typical steroid side effects. Understanding the right loteprednol dosage is key to getting relief without over‑using a steroid.
Topical steroids, medications applied to the surface of skin or eye to reduce swelling and redness work hand‑in‑hand with loteprednol. The dosage you choose depends on the condition being treated, the strength of the preparation, and how long you plan to use it. For example, a 0.5% ophthalmic suspension often requires one to two drops per eye daily for up to two weeks, while a 0.5% cream for dermatitis might be applied two to three times a day for a shorter period. loteprednol dosage therefore reflects the principle that potency must match severity.
Key Factors That Shape the Right Dosage
First, ocular inflammation, conditions like allergic conjunctivitis or post‑surgical eye swelling often need a lower, more frequent dosing schedule to keep the drug in contact with the cornea. Second, skin inflammation, such as atopic dermatitis or psoriasis patches may tolerate a thicker cream applied less often. Third, patient age matters: children and older adults usually start with the minimal effective dose to reduce the risk of cataracts or skin thinning.
These factors create a semantic triple: "Loteprednol dosage" → depends on → "condition severity". Another triple: "Topical steroids" → require → "proper tapering" to avoid rebound inflammation. And a third: "Corticosteroid" → influences → "healing speed" when used correctly.
Third, the form of the medication matters. Loteprednol comes as an ophthalmic suspension, a cream, or a gel. The suspension spreads quickly across the eye surface, so a few drops are enough. In contrast, the cream sits on the skin, needing a thin layer to cover the affected area. The potency of each form is calibrated so that the same active amount delivers comparable anti‑inflammatory power.
Safety tips are part of dosage planning. Always start with the lowest frequency that still controls symptoms. If inflammation persists after five days, a clinician may suggest a short increase in dose, but prolonged high‑dose use raises the chance of side effects like increased intra‑ocular pressure or skin atrophy. For eye use, patients should avoid touching the dropper tip to the eye to prevent contamination.
When you combine loteprednol with other drugs, interactions can shift the effective dose. For instance, using non‑steroidal anti‑inflammatory eye drops alongside loteprednol may enhance healing, allowing a shorter treatment course. However, systemic steroids taken for another condition can amplify the overall steroid load, prompting a clinician to adjust the local dosage.
Finally, follow‑up matters. An eye doctor will usually re‑examine the patient after one week to check pressure and inflammation levels. For skin conditions, a dermatologist may ask for a visual check after two weeks. If the condition clears, tapering the dosage—reducing frequency before stopping—helps maintain results and minimizes rebound.
Our collection below pulls together practical guides, comparison charts, and safety checklists that dive deeper into these topics. Whether you’re looking for a quick dosing cheat‑sheet, a side‑effect warning list, or a step‑by‑step taper plan, you’ll find resources that match the dosage nuances discussed here. Explore the articles to fine‑tune your loteprednol regimen and stay ahead of any issues.
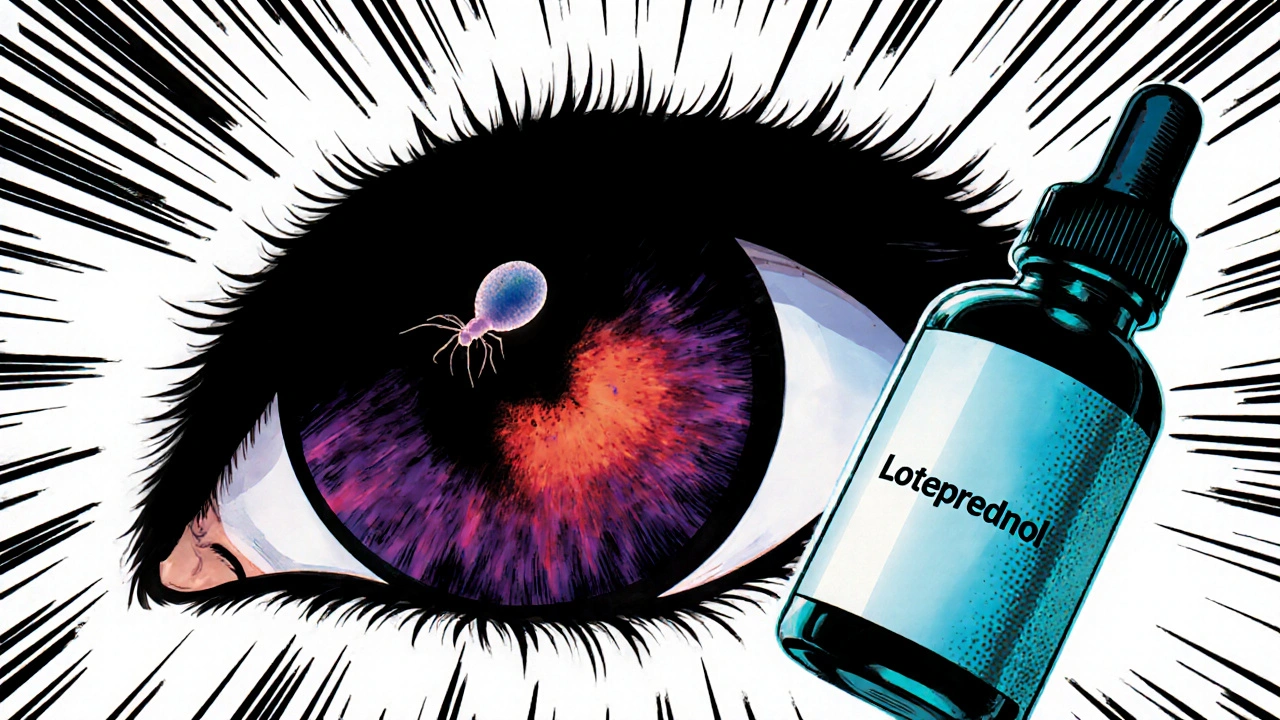
Loteprednol's Role in Managing Ocular Toxoplasmosis
Learn how loteprednol works, dosing guidelines, safety checks, and evidence for treating ocular toxoplasmosis, with practical tips and a comparison to other steroids.
Categories
- Medications (69)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



