Lisinopril Alternatives: Safe Options for Controlling Blood Pressure
When working with Lisinopril alternatives, medications or strategies that can replace lisinopril for treating high blood pressure and heart failure. Also known as ACE inhibitor substitutes, they aim to lower systolic and diastolic readings while offering different side‑effect profiles.
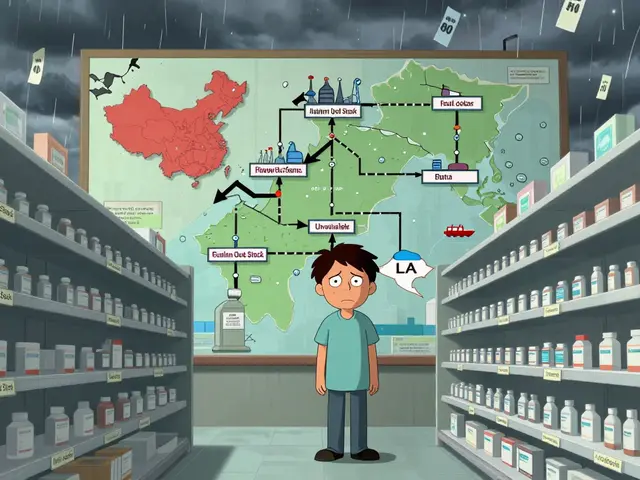
One major group you’ll encounter is Angiotensin II Receptor Blockers (ARBs), drugs like losartan, valsartan, and irbesartan that block the same hormonal pathway as lisinopril but avoid cough and angioedema in many patients. ARBs encompass the same renin‑angiotensin system target, yet they bind to the receptor instead of inhibiting the enzyme. Choosing an ARB often requires checking kidney function because the drugs are cleared renally, establishing a semantic link: Lisinopril alternatives require kidney‑function assessment. Another class, Calcium Channel Blockers, such as amlodipine and diltiazem, relax vascular smooth muscle and reduce cardiac workload, provides a different mechanism that can be paired with or replace an ACE inhibitor. These agents influence blood‑pressure control by preventing calcium influx, which is useful when patients have peripheral edema from ACE inhibitors. A third option, Thiazide Diuretics, including hydrochlorothiazide and chlorthalidone, promote sodium loss and decrease plasma volume, often serves as a first‑line or add‑on therapy. Thiazides require periodic electrolyte monitoring, tying back to the broader need for safety checks across all alternatives.
How to Pick the Right Replacement
Evaluating Lisinopril alternatives starts with a clear picture of your health goals, current lab results, and any side effects you’ve experienced. If a dry cough or facial swelling has made lisinopril hard to tolerate, an ARB usually fits the bill because it sidesteps the bradykinin buildup that triggers those symptoms. If you need stronger vasodilation without affecting the renin‑angiotensin axis, calcium channel blockers might be the answer, especially for patients with concurrent angina. When fluid retention is a concern, thiazide diuretics can shave off excess volume while keeping costs low. Beyond drug classes, lifestyle tweaks act as non‑pharmacologic alternatives. Regular aerobic exercise, a DASH‑style diet low in sodium, and stress‑reduction techniques can cut systolic pressure by 5–10 mmHg, sometimes allowing a lower medication dose or a switch to a milder agent. This connection—lifestyle changes influence the choice of lisinopril alternatives—highlights that medication isn’t the sole player. In practice, doctors often layer two or three of these options to hit target numbers without over‑relying on a single drug. For example, an ARB paired with a low‑dose thiazide can balance efficacy and side‑effect risk. Your clinician will also weigh comorbidities: diabetes, chronic kidney disease, or a history of heart attack each tips the scale toward a specific alternative. Below you’ll find a curated collection of articles that dive deeper into each drug class, compare costs, outline dosing tricks, and share real‑world experiences. Whether you’re switching because of side effects, looking for a cheaper generic, or just curious about how these therapies stack up, the posts ahead give practical, step‑by‑step guidance to help you make an informed decision.
Compare Hypernil (Lisinopril) with Alternatives - A Detailed ACE Inhibitor Guide
A comprehensive guide comparing Hypernil (lisinopril) with other blood pressure meds, covering dosage, cost, side effects, and safe switching tips.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)