Eye Inflammation Treatment: Quick Relief and Long‑Term Care
When dealing with eye inflammation treatment, a set of medical and home‑care steps that reduce swelling, redness, and discomfort in the eyes, the first thing to understand is what’s actually causing the inflammation. Most often you’ll run into bacterial eye infection, an infection usually triggered by staph or strep bacteria that leads to painful red eyes and discharge. When bacteria are the culprit, antibiotic eye drops, medications applied directly to the eye to kill the offending microbes become the frontline cure. In other cases, allergies or dry‑eye stressors spark the problem, and you’ll need antihistamine or lubricating drops instead. eye inflammation treatment therefore covers a range of approaches, each matched to the underlying trigger.
Key Treatment Options and How They Work
One core principle is that eye inflammation treatment requires a correct diagnosis, because using the wrong type of drop can linger the issue or make it worse. If bacteria are identified, prescription antibiotic eye drops—like tobramycin or ciprofloxacin—stop the infection in a day or two. For non‑infectious swelling, corticosteroid eye drops reduce immune response, while non‑steroidal anti‑inflammatory drops (NSAIDs) ease pain without the steroid side‑effects. Ocular allergies, a frequent but often overlooked cause, respond best to antihistamine or mast‑cell stabilizer drops that block the histamine release that makes eyes itchy and watery. Warm compresses and proper eyelid hygiene also support recovery by unclogging blocked glands and flushing out irritants. Seasonal changes matter, too; pollen peaks in spring can aggravate allergic conjunctivitis, so switching to a stronger antihistamine drop during those months is a smart preventive move.
Beyond drops, lifestyle tweaks boost any ocular allergies, allergic reactions that affect the eye surface and cause redness, itching, and tearing management. Keeping windows closed on high‑pollen days, using air filters, and rinsing eyes with sterile saline can cut exposure. If you wear contact lenses, a brief hiatus while the eye heals prevents further irritation. For dry‑eye contributors, artificial tears or omega‑3 supplements keep the tear film stable, reducing the inflammatory cycle. And remember, if symptoms persist beyond 48‑72 hours, worsen, or are accompanied by vision changes, it’s time to see an eye doctor—delayed treatment can lead to complications like corneal ulcers.
Putting it all together, the collection of articles below walks you through specific scenarios: from the seasonal pattern of bacterial eye infections to the safest ways to buy generic medication online, the differences between eye‑drop types, and step‑by‑step home‑care tips. Whether you’re tackling a sudden redness after a hike or managing chronic allergic itch, you’ll find clear, actionable advice that fits your situation.
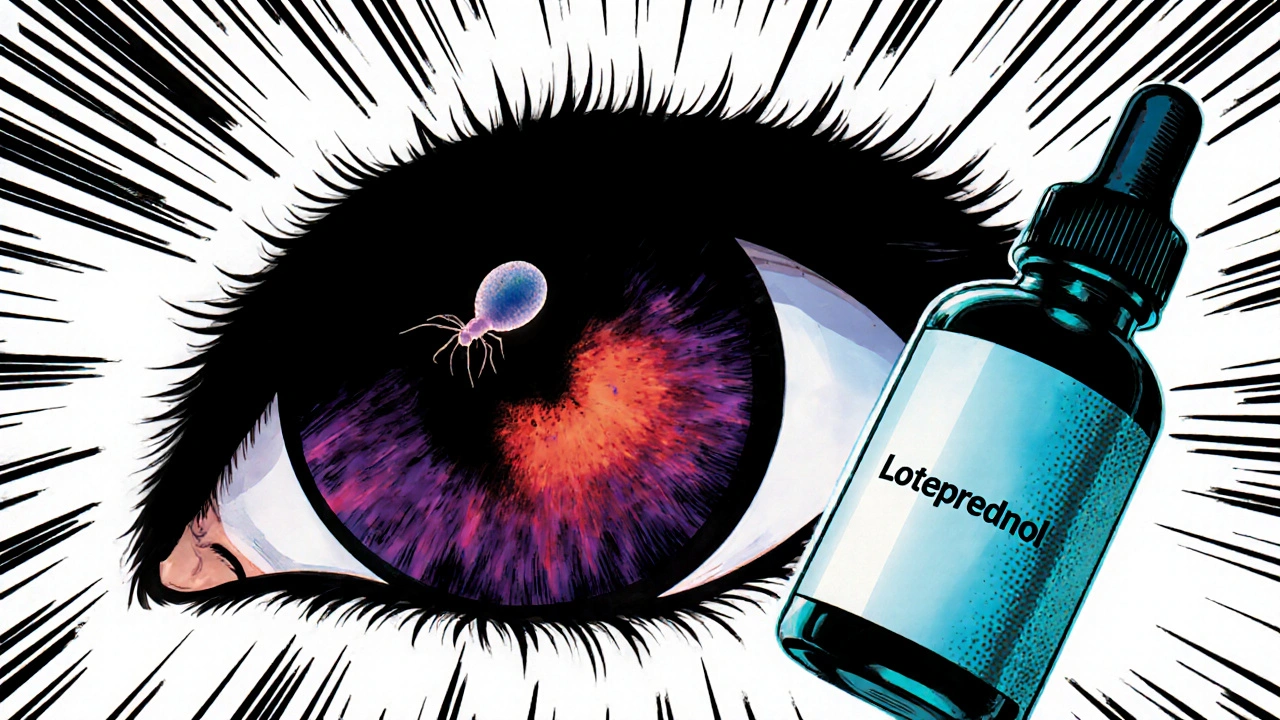
Loteprednol's Role in Managing Ocular Toxoplasmosis
Learn how loteprednol works, dosing guidelines, safety checks, and evidence for treating ocular toxoplasmosis, with practical tips and a comparison to other steroids.
Categories
- Medications (69)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)
Popular Articles