Dasatinib Drug Interactions in Older Patients
When working with Dasatinib drug interactions in older patients, the study of how Dasatinib mixes with other medicines in people over 65. Also known as Dasatinib interactions elderly, it helps clinicians avoid harmful side effects and keep therapy effective.
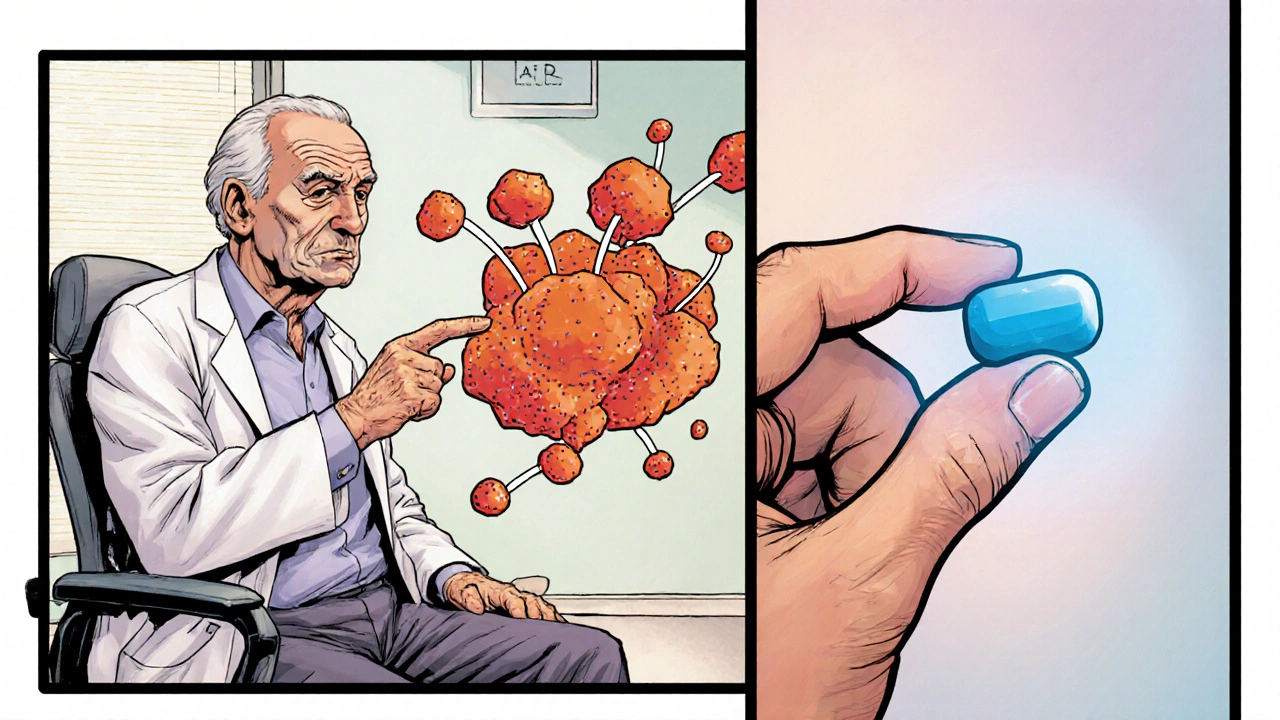
First, understand the drug itself. Dasatinib, a second‑generation tyrosine kinase inhibitor used mainly for chronic myeloid leukemia (CML) blocks the BCR‑ABL protein that drives cancer cells. It belongs to the broader class of tyrosine kinase inhibitors, medicines that interrupt cell signaling pathways in various cancers. Knowing the drug class matters because many TKIs share metabolism routes and similar interaction risks.
The heart of most interactions is the liver enzyme CYP3A4, the primary enzyme that breaks down Dasatinib. Anything that blocks CYP3A4 can raise Dasatinib levels, while strong inducers can drop them below therapeutic range. Older adults often take several drugs—a situation called polypharmacy, the concurrent use of multiple prescription or over‑the‑counter medications—so the chance of hitting CYP3A4 increases dramatically.
Age‑related changes add another layer. Kidney function typically declines after 60, and liver blood flow can slow down, both of which affect how quickly Dasatinib clears. Because the drug has a narrow therapeutic window, even modest shifts in clearance can cause toxicity (like severe fluid retention) or loss of disease control. Adjusting the dose based on creatinine clearance or liver function tests becomes essential for safety.
Common Culprits and How to Spot Them
Dasatinib drug interactions often involve antifungal agents such as ketoconazole, macrolide antibiotics like clarithromycin, and certain HIV protease inhibitors. These drugs are strong CYP3A4 inhibitors and can push Dasatinib concentrations up 2‑3 fold. On the flip side, drugs like rifampin or St. John’s wort can pull levels down, risking disease relapse. Cardiovascular medicines—especially calcium channel blockers (e.g., amlodipine) and certain antihypertensives—may also interact, leading to exaggerated blood pressure drops or increased bleeding risk when combined with Dasatinib’s platelet effects.
Practical steps for clinicians and patients include: 1) creating a complete medication list at every visit, 2) checking for CYP3A4‑modulating drugs before starting or changing Dasatinib, 3) monitoring blood counts, liver enzymes, and fluid status regularly, and 4) adjusting the dose or switching to an alternative TKI when high‑risk interactions are unavoidable. Patient education is key; seniors should be encouraged to report new over‑the‑counter products, herbal supplements, or diet changes that could affect metabolism.
By keeping an eye on enzyme pathways, organ function, and the broader picture of polypharmacy, you can reduce adverse events while preserving the anti‑leukemia power of Dasatinib. Below you’ll find a curated set of articles that dive deeper into specific interaction scenarios, dosing tips for the elderly, and real‑world case studies that illustrate how to apply these principles in everyday practice.
Dasatinib and the Elderly: Key Considerations for Older Patients
A practical guide on using Dasatinib for older patients, covering dosage tweaks, side‑effect management, drug interactions, and monitoring tips tailored to seniors.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)
Popular Articles