Antihistamines: Fast Allergy Relief & How to Use Them Safely
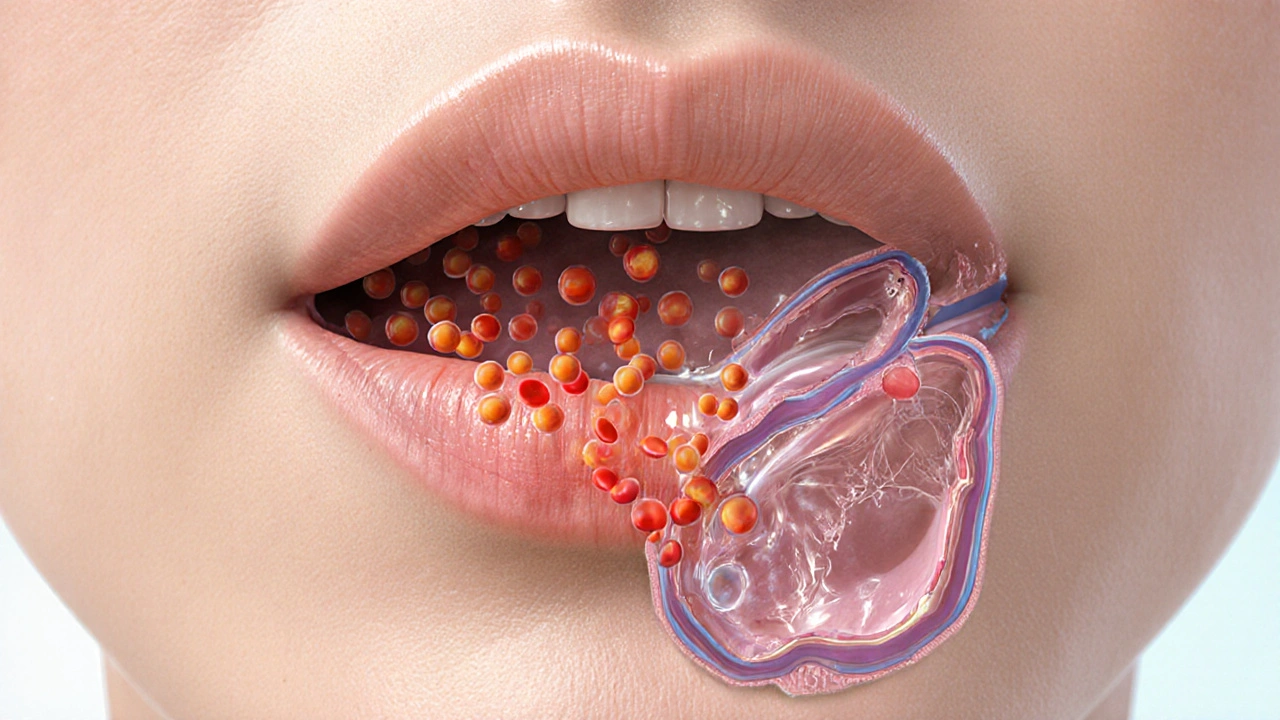
If seasonal sniffles, itchy eyes, or hives sneak up on you, antihistamines are often the first thing people reach for. These medicines block histamine, a chemical your body makes during an allergic reaction. Some act fast and make you sleepy; others relieve symptoms with little or no drowsiness. Know which one fits your life.
Most people choose between first‑generation and second‑generation antihistamines. First‑generation drugs like diphenhydramine (Benadryl) work quickly but cross into the brain and cause drowsiness. That makes them useful at night or for short-term relief, but risky for driving or operating machines. Second‑generation options such as loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are less sedating and last longer—good for daily use.
How to choose the right antihistamine
Think about your daily routine and symptoms. If you need relief during the day and must stay alert, pick a non‑sedating, second‑generation antihistamine. If sleep or short bursts of relief are the goal, a first‑generation medicine at bedtime can help. For itchy or watery eyes, eye drops are often faster and reduce systemic side effects.
Children and dosing: Use age‑specific formulations and follow dosing on the label or directions from your healthcare provider. Many liquid versions exist; never give adult doses to a child. Pregnant or breastfeeding people should check with their clinician before starting any antihistamine.
Safety tips and when to see a doctor
Common side effects include dry mouth, mild drowsiness, and sometimes dizziness. Avoid mixing sedating antihistamines with alcohol or other sedatives. If you take other medications—especially certain antidepressants, blood pressure drugs, or seizure medicines—ask a pharmacist about interactions. If symptoms suggest a severe allergic reaction—trouble breathing, swelling of the face or throat, fainting—call emergency services immediately. Antihistamines can help mild to moderate reactions but are not a substitute for epinephrine in anaphylaxis.
Extra tips for everyday control
Combine antihistamines with nasal steroid sprays for better control of nasal symptoms. Track triggers and match your prevention plan—start daily meds a week before high‑pollen seasons for best results. If OTC options fail after a few weeks, see an allergist; testing and targeted treatments like immunotherapy could offer long‑term relief.
Generic vs brand names: generic antihistamines contain the same active drug as brands but usually cost less. Look for the active ingredient on the label—diphenhydramine, loratadine, cetirizine, or fexofenadine—so you know what you are buying.
Avoid combining oral antihistamines with decongestant combinations unless needed; decongestants raise blood pressure and can cause jitteriness. If you must use a combination pill, check with a pharmacist about existing health issues and timing.
Long‑term daily use is safe for many people with seasonal or chronic allergies, but review this with your doctor every year. Some people notice tolerance to sedation effects, not loss of allergy control.
Use antihistamines with a plan: pick the right type, follow dosing rules, and check interactions. That keeps symptoms down and life moving.
Keep an allergy log to spot triggers and medication patterns. It really helps. Often.
How Histamine Triggers Angioedema: Causes, Symptoms, and Treatment
Learn how histamine triggers angioedema, how to spot it, and the best treatments. Get clear differences from bradykinin‑mediated swelling and practical prevention tips.

9 Alternatives to Atarax for Allergy and Itching Relief
Explore effective alternatives to Atarax for managing allergies and itching, each with distinct advantages and disadvantages. This article will help you understand the various antihistamine options available, offering insights into their effectiveness and potential side effects. Whether you seek moderate sedation or less drowsiness, these alternatives provide varied choices to suit individual needs.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)



