Switching Medications: Proven Strategies to Reduce Side Effects and Avoid Withdrawal
Medication Switching Calculator
Switching medications isn’t just about swapping one pill for another. It’s a delicate process that can trigger everything from mild nausea to life-threatening reactions if done wrong. Too many people are told to stop one drug and start another the next day-only to end up with brain zaps, insomnia, dizziness, or worse. The truth? medication switching needs a plan. Not guesswork. Not convenience. A real, science-backed strategy tailored to your body and your meds.
Why Do Side Effects Happen During Switches?
Your brain adapts to the meds you take. Over time, it changes how it produces and uses neurotransmitters like serotonin, norepinephrine, or dopamine. When you suddenly remove that drug, your brain doesn’t snap back instantly. It stumbles. That’s when withdrawal kicks in. Symptoms like brain zaps, sweating, anxiety, or flu-like feelings aren’t in your head-they’re biological. And they’re common. Studies show 24% to 80% of people experience them, depending on the medication. For SSRIs like sertraline or escitalopram, it’s often 60% or higher. The bigger problem? Doctors often don’t talk about this until after you’re already feeling awful. A 2022 survey found that only 43% of primary care doctors follow optimal switching protocols. That means more than half of patients are being switched without the safety nets they need.The Four Main Ways to Switch (And Which One Works Best)
There are four standard methods for switching medications. Each has pros, cons, and ideal use cases. Knowing which one fits your situation can mean the difference between a smooth transition and a hospital visit.- Direct Switch: Stop the old drug. Start the new one the next day. Simple. Fast. Risky. This works best when switching between drugs in the same class-like from one SSRI to another. Success rates hit 92% in those cases. But if you’re jumping from an SSRI to an SNRI like venlafaxine, your risk of serotonin syndrome jumps 37%. That’s when your body gets flooded with too much serotonin. Symptoms: high fever, fast heartbeat, confusion, muscle rigidity. It’s rare-but deadly if missed.
- Conservative Switch: Taper the old drug slowly, then wait 3 to 5 half-lives before starting the new one. This gives your body time to reset. For drugs with long half-lives like fluoxetine (Prozac), that’s a 25- to 30-day gap. For shorter-acting ones like paroxetine (Paxil), 3 to 5 days. This method cuts side effects by 41% compared to direct switching. But it comes with a trade-off: your risk of relapse goes up by 22% during the drug-free window. Not ideal if you’re struggling with depression or anxiety.
- Moderate Switch: A middle ground. Taper the old med, wait just 2 to 4 days, then start the new one. It’s the most common approach in clinics because it’s easy to schedule. But it fails with short-half-life drugs like venlafaxine or duloxetine. In one study, only 54% of patients had a smooth transition using this method for those meds.
- Cross-Taper: This is the gold standard. You slowly reduce the old drug while slowly increasing the new one. Over 7 to 14 days, the balance shifts. This works best when switching between different classes-say, from an SSRI to an SNRI or even from an SSRI to bupropion. Sixty-three percent of clinicians prefer it. Why? Because it keeps your neurotransmitter levels stable. A 2023 study showed 78% of patients had fewer symptoms using cross-tapering. One user on GoodRx wrote: “Gradually reducing Lexapro while introducing Zoloft over 10 days eliminated the nausea and dizziness I’d experienced with previous abrupt switches.”
What Your Medication’s Half-Life Tells You
The half-life of a drug is how long it takes for half of it to leave your system. This isn’t just a chemistry term-it’s your roadmap. If you ignore it, you’re flying blind.- Fluoxetine (Prozac): Half-life of 4 to 6 days. That means it sticks around for weeks. You can’t just stop it and start something else next week. You need a 25- to 30-day washout. Trying to rush this can cause lingering side effects or interactions.
- Paroxetine (Paxil), Venlafaxine (Effexor): Half-life under 24 hours. These leave your system fast. That’s why people feel withdrawal so quickly-sometimes within hours. Tapering is critical. Abrupt stops here cause severe dizziness, electric shock sensations, and vomiting.
- Escitalopram (Lexapro), Sertraline (Zoloft): Half-life around 27-32 hours. Moderate. A 5- to 7-day taper usually works well with cross-tapering.
Who’s at Highest Risk?
Not everyone switches the same way. Some people are more vulnerable. If any of these apply to you, you need extra caution.- People over 65: Their bodies process drugs slower. Withdrawal symptoms are 2.3 times more severe than in younger adults. Dizziness or confusion can lead to falls. Slower tapers are non-negotiable.
- Those switching from MAOIs: Monoamine oxidase inhibitors (like phenelzine or tranylcypromine) are powerful. Switching to an SSRI without a full 14-day washout can cause a hypertensive crisis-blood pressure spikes that can cause stroke or heart attack. This isn’t a risk you take lightly.
- People with a history of withdrawal: If you’ve had bad reactions before, your brain is more sensitive. Cross-tapering isn’t optional-it’s essential.
- Those on multiple psychiatric meds: Polypharmacy increases interaction risk. Adding a new drug while still on others can trigger unexpected side effects. Always review all meds with a pharmacist.
What to Do Before You Switch
A good switch starts before you even get the new prescription. Here’s your checklist:- Get your full medication history: List every drug you’ve taken in the last 2 years-even ones you stopped. Include doses and how long you took them. This helps your doctor spot patterns.
- Check your half-life: Use a reliable source like the Specialist Pharmacy Service’s switching guide or GoodRx’s clinical charts. Don’t rely on memory.
- Use the DASS checklist: The Discontinuation Emergent Signs and Symptoms scale helps predict who’s likely to have trouble. Ask your doctor if they’ve used it.
- Plan your taper: Don’t wing it. Ask for a written schedule: “Week 1: reduce by 25%. Week 2: reduce by another 25%. Start new med at 25mg on Day 8.”
- Set up follow-ups: Schedule check-ins at 3, 7, and 14 days after the switch. Withdrawal symptoms often peak between days 3 and 5. You need someone to talk to if things go sideways.
What to Do If Things Go Wrong
Even with the best plan, side effects can pop up. Here’s what works:- Brain zaps? These electric-shock sensations are common with SSRIs. They usually fade within days. If they’re severe, your doctor might temporarily add a low dose of hydroxyzine or a short-acting benzodiazepine like lorazepam-just to get you through.
- Insomnia or anxiety? Melatonin (1-3mg at night) helps many. Avoid caffeine. If it’s intense, a 1- to 2-week course of low-dose trazodone can help reset sleep without dependency.
- Nausea or dizziness? Ginger supplements or peppermint tea help some. If it’s persistent, your doctor might prescribe ondansetron (Zofran) for a few days.
- Worse mood or panic attacks? This could mean the new drug isn’t working yet-or you’re having withdrawal. Don’t stop it. Call your doctor. You might need to slow the taper or adjust the dose.
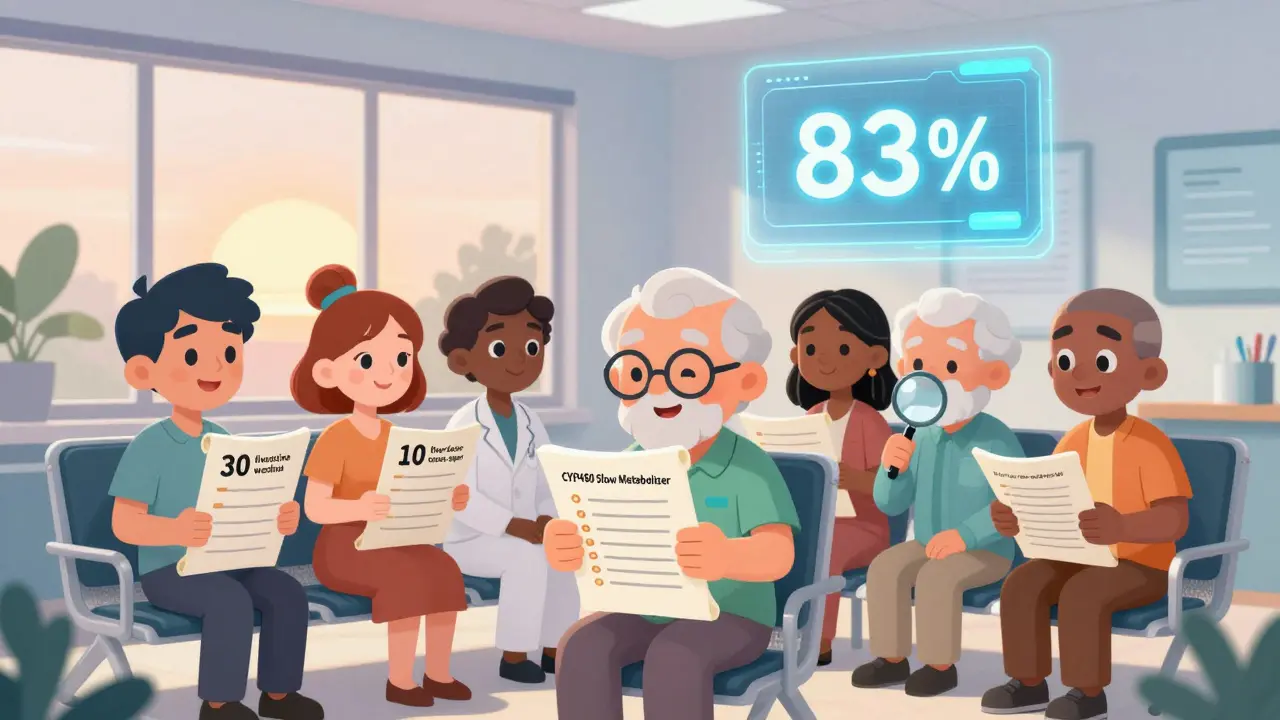
The Future Is Personalized
We’re moving beyond one-size-fits-all switching. New tools are emerging:- AI-driven tools: Google Health’s algorithm, trained on 1.2 million patient records, can now predict the best switch with 83% accuracy. It considers your age, meds, genetics, and past reactions.
- Genetic testing: Some clinics now test for CYP450 enzyme variants. If you’re a slow metabolizer, you need lower doses. One 2022 study showed 33% better outcomes when switching was guided by genetics.
- EEG biomarkers: UCLA researchers found brainwave patterns that predict who will tolerate a switch well. It’s not mainstream yet-but it’s coming.
- VA’s new system: Since January 2024, the U.S. Veterans Health Administration has integrated a switching decision aid into its EHR. It’s already projected to prevent 12,500 adverse events a year.
What to Ask Your Doctor
Don’t leave your switch to chance. Use these questions to guide the conversation:- “What’s the half-life of my current medication?”
- “Which switching method do you recommend, and why?”
- “What symptoms should I watch for in the first week?”
- “Do I need a bridge medication like hydroxyzine or bupropion?”
- “Can you give me a written taper schedule?”
- “When should I call you if things get worse?”
Final Thought: You’re Not Alone
Switching meds is one of the most stressful things you can do in your health journey. But it doesn’t have to be a gamble. With the right plan, most people make it through with little to no trouble. The key is preparation, patience, and asking the right questions. You’re not just taking a pill-you’re guiding your brain back to balance. Do it right, and you’ll feel better faster. Do it wrong, and you might lose weeks-or worse.Can I switch antidepressants without tapering?
Technically, yes-but it’s risky. Abruptly stopping SSRIs or SNRIs causes withdrawal symptoms in 60% of people. Brain zaps, nausea, dizziness, and anxiety are common. For drugs with short half-lives like paroxetine or venlafaxine, symptoms can start within hours. Tapering reduces these risks by up to 41%. Only direct switches between similar drugs (like one SSRI to another) are sometimes safe without tapering, and even then, it’s not recommended.
How long does it take to feel better after switching?
It varies. Withdrawal symptoms usually peak between days 3 and 5 and fade within 1 to 2 weeks. But the new medication typically takes 4 to 6 weeks to reach full effect. Don’t expect immediate results. If you’re still feeling awful after 3 weeks, talk to your doctor. You might need a dose adjustment or a different drug.
Is cross-tapering better than stopping one drug first?
For most people, yes-especially when switching between different drug classes. Cross-tapering keeps your brain chemistry stable by overlapping the drugs. Studies show 78% of patients have fewer side effects this way. Stopping first creates a gap where withdrawal hits hard. The only exception is when the old drug has a very long half-life (like fluoxetine), where a washout is safer than overlapping.
Can switching meds cause serotonin syndrome?
Yes, especially if you switch from an SSRI or SNRI to another serotonergic drug too quickly-or if you’re on multiple drugs that increase serotonin. Risk is highest when switching from MAOIs to SSRIs without a 14-day washout. Symptoms include fever, rapid heart rate, confusion, muscle stiffness, and tremors. It’s rare (0.5-1.7 cases per 1,000 patient-years) but can be life-threatening. Always tell your doctor every medication you’re taking.
Should I get genetic testing before switching?
It’s not required, but it can help. If you’ve had bad reactions to multiple antidepressants, genetic testing for CYP450 enzymes can show if you metabolize drugs slowly or quickly. One study found 33% better outcomes when switches were guided by genetics. It’s not covered by all insurance, but it’s worth considering if you’ve struggled with medication changes before.






Allen Ye
January 4, 2026 AT 15:28Look, I get that this is supposed to be a guide, but honestly? This reads like a pharmaceutical whitepaper that got lost in a TED Talk. The science is solid-half-lives, cross-tapers, serotonin syndrome thresholds-but nobody’s talking about the real issue: the system is broken. Doctors are overworked, underpaid, and trained to treat symptoms, not people. You want to switch meds? Good luck getting a 30-minute appointment where they actually listen. I’ve been through three switches. Two of them ended with ER visits because no one bothered to check my history or explain the timeline. The algorithm they mentioned? It’s great-if you’re in a VA hospital or a Silicon Valley clinic. For the rest of us? We’re just guinea pigs with insurance cards. The real innovation isn’t in genetics or EEGs-it’s in forcing healthcare to stop treating patients like disposable data points.
mark etang
January 4, 2026 AT 18:09Thank you for this meticulously researched and clinically sound exposition on the pharmacological nuances of medication transition protocols. The structural integrity of your methodology, particularly the delineation of half-life-dependent tapering windows and the empirical validation of cross-tapering efficacy, represents a paradigmatic advancement in patient-centered psychiatric care. It is imperative that primary care providers integrate these evidence-based frameworks into standard clinical practice to mitigate iatrogenic harm. I urge all stakeholders-clinicians, administrators, and policymakers-to adopt these guidelines without delay.
Michael Rudge
January 5, 2026 AT 17:30Wow. So you wrote a 2,000-word essay to tell people to ‘ask their doctor’? Groundbreaking. I’m sure the 80% of patients who get prescribed meds by a 6-minute telehealth visit are just dying to hear about ‘half-lives’ and ‘CYP450 enzymes.’ Meanwhile, my cousin’s mom got switched from sertraline to fluoxetine and spent three days screaming in the bathroom because her doctor said ‘it’s the same thing.’ You think your 78% success rate matters when the system’s designed to churn out prescriptions like fast food? Congrats-you turned a life-or-death process into a quiz show. Now go tell that to the person on Medicaid who can’t afford a psychiatrist who knows what ‘washout’ means.
Ethan Purser
January 7, 2026 AT 06:28Bro. I just wanna say… this post hit me right in the soul. 😭 I switched from Lexapro to Zoloft last year and it felt like my brain was being rewired by a drunk intern. The brain zaps? Yeah. I swear I heard my neurons screaming. I cried in the shower for a week. But then I found this guy on Reddit who said to take magnesium and breathe through your nose and… I don’t know, something shifted. I’m not fixed. I’m not ‘healed.’ But I’m here. And I’m not alone. If you’re reading this and you’re in the middle of that hell-breathe. You’re not crazy. Your brain is just adjusting. And it’s gonna be okay. I promise. 🌱
Doreen Pachificus
January 8, 2026 AT 06:59Interesting. I’ve been on the same SSRI for 7 years and my doctor just said ‘you’re fine, keep taking it.’ No mention of half-lives, no taper plan. I wonder if I’ve been quietly accumulating withdrawal symptoms this whole time. Maybe that’s why I get dizzy when I stand up too fast. Or why I’ve been having these weird ‘electric’ dreams. Huh. Guess I’ll google my med’s half-life now.
Cassie Tynan
January 9, 2026 AT 11:22Oh please. ‘Cross-tapering is the gold standard.’ Yeah, right. Like that’s gonna happen in a clinic where the nurse hands you a 30-day script and says ‘call if you feel weird.’ I’ve been through two switches. First time: I was suicidal for a month. Second time: I took a week off work and just sat on my couch crying while watching The Office on loop. And guess what? My doctor didn’t even ask if I was okay. She just upped the dose. So yeah, ‘78% fewer symptoms’-great. But that’s not the reality for most of us. The real gold standard? A doctor who gives a damn. And that’s rarer than a functioning mental health system.
Rory Corrigan
January 11, 2026 AT 05:57Just saying… 🤔 maybe the problem isn’t the meds. Maybe it’s that we’re trying to fix existential loneliness with chemistry. I get the science. I do. But what if the real ‘half-life’ we need to taper is our dependence on pills to feel human? I’m not saying ditch the meds. I’m saying… maybe we need to ask bigger questions. Like: why are we so broken that we need to rewire our brains just to get through Tuesday? 🌿
Jack Wernet
January 12, 2026 AT 15:56This is an exceptionally thorough and well-structured overview of pharmacological transition protocols. The inclusion of clinical data, patient-reported outcomes, and emerging technological interventions provides a comprehensive foundation for informed decision-making. I commend the author for emphasizing patient agency and the necessity of physician accountability. Such resources are desperately needed in primary care settings where time constraints often compromise optimal care. I will be sharing this with my colleagues in the psychiatry department.
Uzoamaka Nwankpa
January 12, 2026 AT 23:45I don't know why people make it so complicated. In Nigeria, we just take the new medicine and hope. If you feel bad, you drink ginger tea. If you feel worse, you go to the church. They pray. Sometimes it works. Sometimes you just live with it. I think the problem is not the medicine. The problem is we think we can control everything with science. Maybe we just need to be still and wait. God knows what our body needs.
Chris Cantey
January 14, 2026 AT 05:14I read this whole thing and all I could think was: how many people died because someone didn’t know the half-life of venlafaxine? The fact that this is even a question is terrifying. We’ve turned human neurochemistry into a math problem and then outsourced the solution to a doctor who’s got 12 patients lined up and a 10-minute window. I’ve seen friends go from ‘I’m fine’ to ‘I can’t move’ in 48 hours because they were told to ‘just switch.’ This isn’t medicine. It’s Russian roulette with SSRIs. And the worst part? No one gets punished for it.
Terri Gladden
January 15, 2026 AT 19:44OMG I JUST SWITCHED AND I’M DYING!!! BRAIN ZAPS EVERY TIME I BLINK!!! I TOOK ZOLOFT AND STOPPED LEXAPRO AND NOW I CAN’T SLEEP AND I FEEL LIKE I’M FALLING THROUGH A TUNNEL!! I READ THIS AND I’M LIKE OH SHIT I DID IT WRONG!! I NEED A DOCTOR I NEED A DOCTOR I NEED A DOCTOR!!