Pricing Pressure and Shortages: How Supply Chain Crises Are Reshaping Health Costs
When you walk into a pharmacy and find your usual prescription out of stock, or your doctor tells you the new medication you need won’t be available for months, it’s not just bad luck. It’s the result of pricing pressure and shortages that have been reshaping health economics since 2020. These aren’t temporary hiccups-they’re structural shifts with real consequences for patients, providers, and the entire system.
Why Medications Disappear and Prices Spike
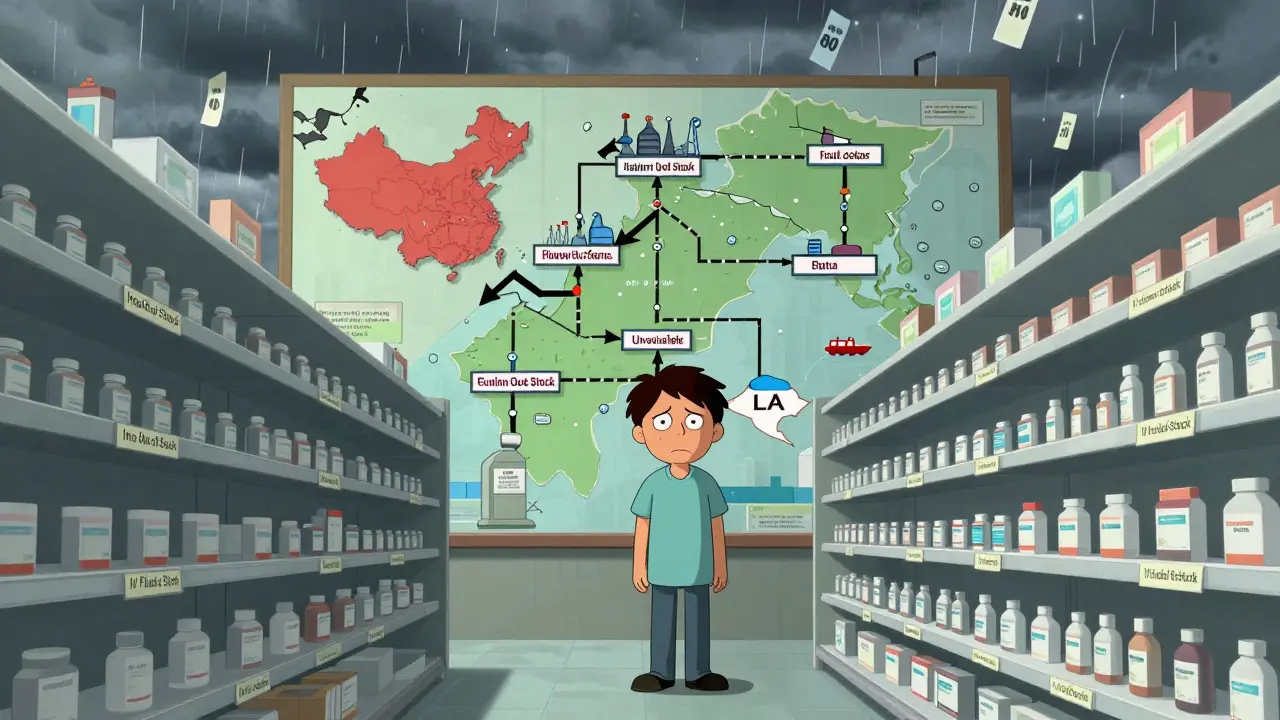
It starts with supply chains. A single pill can pass through eight or more countries before it reaches your hands. Active pharmaceutical ingredients often come from India or China. Packaging materials come from Europe. Finished products are assembled in the U.S. or Canada. When one link breaks-say, a factory in Shanghai shuts down due to lockdowns, or a shipping port in Los Angeles backs up-the whole system trembles. By late 2021, over 70% of U.S. hospitals reported shortages of at least one essential drug, according to the American Society of Health-System Pharmacists. Insulin, antibiotics, chemotherapy agents, even basic IV fluids vanished from shelves. Why? Because demand surged as pandemic care expanded, while production capacity couldn’t keep up. At the same time, energy prices spiked. Making drugs is energy-intensive. When natural gas prices in the UK hit £200 per therm-five times the five-year average-pharmaceutical manufacturers faced sudden cost hikes of 25-40%. These aren’t abstract numbers. They translate into real price jumps. Between 2020 and 2022, the cost of 10 of the most commonly prescribed generic drugs rose by an average of 32%. Some, like metformin for diabetes, doubled in price. The Federal Reserve found that supply chain disruptions alone accounted for nearly 60% of the inflation spike in U.S. goods during that period-and healthcare goods were among the hardest hit.Shortages Don’t Just Mean ‘Out of Stock’
A shortage isn’t just when a shelf is empty. It’s when you have to wait weeks for a refill, switch to a less effective alternative, or skip doses because you can’t afford the new price. In 2022, 58% of U.S. consumers said they’d been unable to buy something they needed due to shortages. For health products, that number was higher. Patients with chronic conditions like hypertension, diabetes, or asthma were hit hardest. One study showed that 1 in 4 patients with type 2 diabetes delayed filling prescriptions during the peak shortage period. That’s not just inconvenient-it’s dangerous. Missed doses lead to hospitalizations, which cost the system far more than the drug itself. Even when drugs are available, they’re often rationed. Pharmacies began limiting refills to 30-day supplies. Doctors started prescribing lower doses to stretch inventory. Some patients turned to online pharmacies with unregulated suppliers. The FDA reported a 40% increase in counterfeit drug seizures between 2020 and 2023, directly tied to desperation caused by shortages.Price Controls Make Things Worse
Governments tried to fix this by capping drug prices. Canada and the UK imposed price controls to protect patients. But in the U.S., where prices are mostly market-driven, manufacturers responded by cutting supply to avoid losses. A 2022 analysis by the Office for Budget Responsibility showed that when price caps prevented companies from raising prices to cover rising costs, 27 small UK energy suppliers went bankrupt. The same pattern played out in pharmaceuticals. Manufacturers with thin margins-especially those making generic drugs-simply stopped producing. Why make a drug that sells for $5 if the raw materials cost $6? The result? More shortages. The Foundation for Economic Education found that price ceilings don’t reduce prices long-term-they create scarcity. When people expect a shortage, they hoard. A Reddit thread from September 2021 had over 2,400 upvotes describing how families in the UK stockpiled asthma inhalers after hearing rumors of a shortage. That panic buying emptied shelves faster than any supply chain issue could.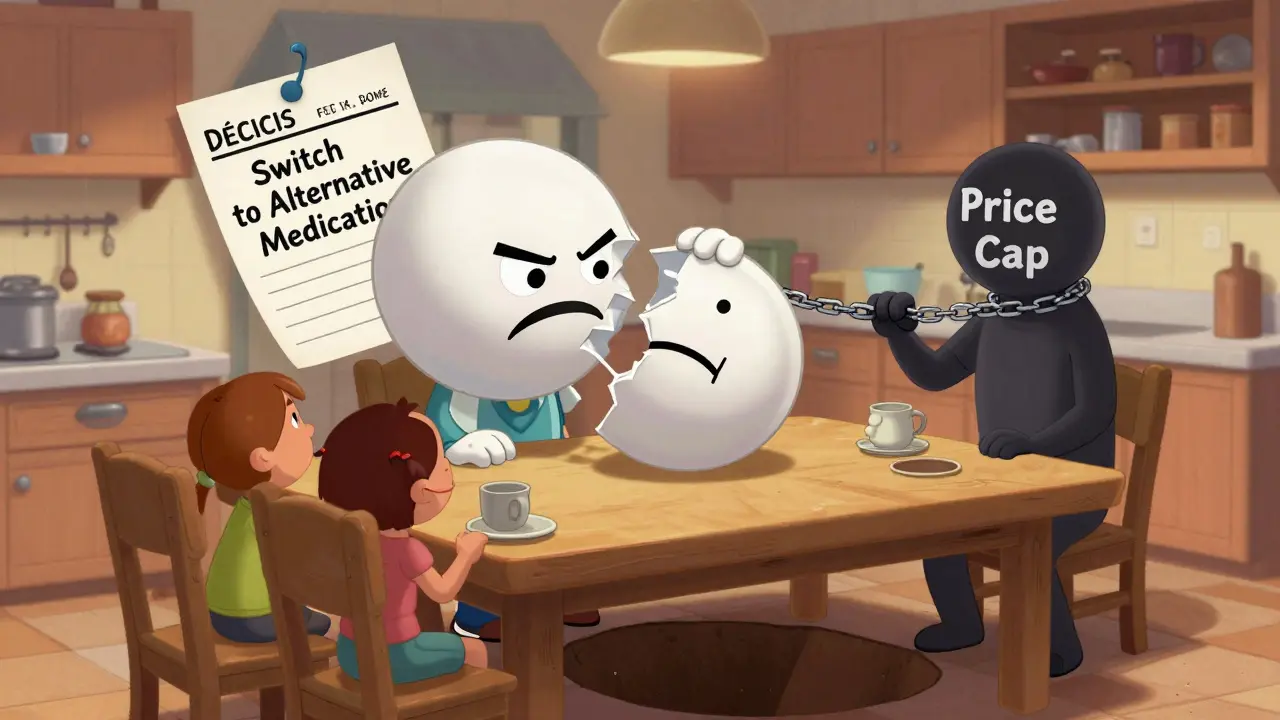
Who Pays the Real Cost?
The biggest myth is that “the system” absorbs these costs. It doesn’t. Patients pay. Employers pay. Taxpayers pay. Insurance companies raised premiums to cover higher drug costs. Between 2021 and 2023, average employer-sponsored health plan premiums jumped 14%-nearly double the pre-pandemic rate. Many patients saw their out-of-pocket costs climb even higher. Deductibles rose. Copays increased. Some plans stopped covering certain generics entirely. Hospitals paid more for the same drugs, then passed those costs on through higher facility fees. A 2023 survey of 300 U.S. hospitals found that 68% increased charges for outpatient services to offset drug supply costs. That’s not inflation-it’s survival. And for low-income patients? The impact was brutal. A 2022 study from the Kaiser Family Foundation found that 34% of adults earning under $30,000 annually skipped medications due to cost or availability. That’s one in three. For seniors on fixed incomes, the numbers were worse.What’s Changing Now?
By early 2023, global supply chain pressure had returned to pre-pandemic levels, according to the San Francisco Federal Reserve’s Global Supply Chain Pressure Index. That’s good news. But don’t assume the problem is solved. The real shift is structural. Companies are no longer chasing “just-in-time” efficiency. They’re building “just-in-case” resilience. A McKinsey survey of 500 global firms found that those using dual-sourcing-buying the same drug ingredient from two different suppliers-recovered from disruptions 35% faster. That’s why we’re seeing more drug manufacturing move to Mexico, India, and even the U.S. The Inflation Reduction Act of 2022 included $1.2 billion to rebuild domestic API production. It’s slow, but it’s happening. Digital tools are helping too. Hospitals are using AI to predict shortages before they happen. One Canadian health network reduced stockouts by 28% using real-time inventory tracking linked to global supplier data. Pharmacies are sharing inventory across regions instead of hoarding locally. The European Central Bank’s 2022 recommendation-temporarily relaxing competition rules to let drugmakers share production capacity-worked. Germany used it to cut pharmaceutical shortages by 19% in six weeks. That kind of cooperation might become standard.
What This Means for You
If you rely on prescription drugs, here’s what you need to know:- Don’t wait until your last pill to refill. Start the process 10-14 days early.
- Ask your pharmacist about alternative brands or formulations. Sometimes a different salt form or delayed-release version is available.
- Check the FDA’s drug shortage database-it’s updated weekly and free to use.
- If you’re on a fixed income, ask about patient assistance programs. Many manufacturers offer them, even for non-covered drugs.
- Consider mail-order pharmacies. They often have better inventory stability than local stores.
The Bigger Picture
This isn’t just about drugs. It’s about how we value health in an economy built on speed and cost-cutting. The pandemic exposed a fragile system. We optimized for profit, not resilience. Now we’re paying the price-in higher costs, longer waits, and worse outcomes. The good news? We’re learning. More countries are investing in domestic production. More companies are diversifying supply chains. More patients are becoming informed advocates for their own care. But the real fix won’t come from policy alone. It’ll come from recognizing that healthcare isn’t a commodity to be traded like oil or wheat. It’s a lifeline. And when lifelines break, everyone suffers.Why are prescription drug prices still rising even though supply chains are improving?
Even as global supply chains stabilize, the cost of making drugs hasn’t gone back to pre-pandemic levels. Energy, labor, and raw materials are still more expensive. Many manufacturers raised prices during the crisis and haven’t lowered them, even when costs eased. Plus, some companies consolidated during the shortage, reducing competition and keeping prices high.
Can the U.S. really produce its own medicines to avoid shortages?
Yes, but it’s expensive and slow. The U.S. currently produces less than 10% of its active pharmaceutical ingredients. Building new facilities takes 5-7 years and costs hundreds of millions. The Inflation Reduction Act is funding domestic production, but it’s a long-term fix. In the short term, nearshoring to Mexico and Canada is helping more quickly.
Are generic drugs more likely to be in short supply than brand-name ones?
Yes. Generic drugs have razor-thin profit margins. When input costs rise, manufacturers often stop making them because they can’t raise prices enough to cover costs. Brand-name drugs, protected by patents, can charge more and absorb cost increases. That’s why shortages hit generics hardest-like metformin, insulin, and antibiotics.
How do supply chain issues affect mental health medications?
They affect them severely. Antidepressants, antipsychotics, and ADHD medications saw some of the worst shortages between 2021 and 2023. Many are made with complex chemical processes and rely on just one or two global suppliers. When those suppliers face delays, patients go without. In 2022, the American Psychiatric Association warned that medication shortages were contributing to increased hospitalizations for mental health crises.
What should I do if my medication is on the FDA’s shortage list?
First, don’t panic. Contact your pharmacist-they may have access to alternative suppliers or formulations. Talk to your doctor about switching to another drug in the same class. Some alternatives work just as well. You can also check the FDA’s Drug Shortages page for updates and manufacturer contacts. If you’re struggling to afford it, ask about patient assistance programs-many drugmakers offer them.
Will inflation return if supply chains break again?
Almost certainly. The Federal Reserve and IMF both warn that future disruptions-whether from climate events, geopolitical conflict, or new pandemics-could push inflation higher again, especially in healthcare. Unlike in 2021, we now know how fragile these systems are. The question isn’t if another shock will happen, but when-and whether we’re ready.




anthony martinez
January 10, 2026 AT 07:21So let me get this straight-we spent two years screaming about supply chains, and now the solution is to make everything more expensive so companies can afford to make the same pills they were making before? Brilliant. Just brilliant.
Meanwhile, my insulin co-pay went up 40% and the pharmacy still can’t guarantee a refill. Thanks, market dynamics.
At this point, I’d rather just brew my own medicine out of tea leaves and hope for the best.
Michael Marchio
January 11, 2026 AT 00:51The entire structure of pharmaceutical pricing is a house of cards built on the illusion of competition. Generic drugs aren’t ‘cheap’-they’re exploited. Manufacturers operate on margins thinner than a sheet of graphene, and when input costs rise-even modestly-they vanish overnight because there’s no incentive to produce something that doesn’t yield a 300% return. Meanwhile, brand-name drugs, protected by patents and lobbying power, hike prices with impunity. This isn’t capitalism-it’s rent-seeking dressed up as free enterprise. The FDA’s shortage list isn’t a symptom of supply chain issues-it’s a direct consequence of deregulation, consolidation, and the abandonment of public interest in favor of shareholder value. We’ve turned healthcare into a casino, and patients are the ones losing their life savings on every spin.
And don’t get me started on how ‘nearshoring’ to Mexico is just outsourcing exploitation to a lower-wage country with weaker environmental controls. The problem isn’t geography-it’s profit motive.
neeraj maor
January 11, 2026 AT 12:29They never tell you the real reason generics are disappearing.
It’s not just cost. It’s not just energy. It’s the Chinese government quietly buying up API manufacturers and stockpiling them for geopolitical leverage. You think this is about profits? No. It’s about control. The U.S. doesn’t make its own medicine because it doesn’t want to-because it’s easier to rely on a regime that could cut off supply at any moment. The FDA’s database? A distraction. The real data is classified. The 2023 spike in counterfeit seizures? That’s just the tip. The black market is thriving because the system is rigged to fail. And now they want to ‘invest in domestic production’? Too little, too late. By the time those plants open, the next pandemic or war will have already severed the next link.
They’re not fixing the system. They’re just moving the chess pieces so the same players still win.
Ritwik Bose
January 11, 2026 AT 13:42Thank you for this deeply thoughtful and well-researched piece. 🙏
It’s heartbreaking to see how our pursuit of efficiency has left so many vulnerable. I’ve seen this firsthand in India-where many generic manufacturers are now prioritizing exports over domestic needs because international buyers pay more. The irony is that the same drugs that save lives in the U.S. are being rationed in the countries that made them.
Perhaps the real solution lies in global cooperation-not just in production, but in fair pricing frameworks that recognize healthcare as a human right, not a commodity. Let’s push for transparency, shared capacity, and ethical sourcing. We can do better.
And yes, I’ll start refilling my meds 14 days early. 😊
Paul Bear
January 13, 2026 AT 04:10Let’s be precise: the issue isn’t ‘pricing pressure’-it’s price elasticity misalignment in a monopolistically competitive market with asymmetric information. Generic manufacturers, operating under thin margins and zero pricing power, exit the market when marginal cost exceeds average revenue. This is basic microeconomic theory. The FDA’s shortage database reflects this equilibrium shift, not supply chain fragility per se.
Moreover, the notion that ‘just-in-case’ inventory is a panacea ignores the capital inefficiency it introduces. Inventory carrying costs alone can add 15–20% to unit cost. The real innovation isn’t dual-sourcing-it’s predictive analytics and dynamic pricing algorithms that incentivize production without distorting demand. And yes, the Inflation Reduction Act’s $1.2B is a band-aid on a hemorrhage. We need a public-private partnership modeled after the Defense Production Act, not a subsidy lottery.
Also, ‘mail-order pharmacies’ are not a solution-they’re a logistical workaround that shifts burden to the patient. The system should adapt, not the patient.
lisa Bajram
January 13, 2026 AT 09:26OMG I JUST REALIZED I’VE BEEN RUNNING ON EMPTY FOR MONTHS 😭
My anxiety med? Gone. My thyroid med? ‘We’ll call you if it comes in.’ I called 7 times. They said ‘it’s a global issue’ like I’m supposed to just sit here and breathe through it while my heart races like a jackhammer.
So I did what any sane person would do-I started asking EVERYONE. My pharmacist? She hooked me up with a different brand. My doctor? She switched me to a liquid form that’s actually available. My sister? She sent me a care package with extra pills she had saved.
And guess what? I found a patient assistance program that gave me 6 months free. It’s not perfect. But it’s a lifeline.
To anyone reading this: DON’T SUFFER IN SILENCE. Ask. Call. Email. Beg. You’re not being a burden-you’re being brave. And you’re not alone. 💪❤️
Jaqueline santos bau
January 13, 2026 AT 16:25Okay but let’s be REAL for a second-this isn’t about supply chains. This is about Big Pharma laughing all the way to the bank while we’re crying in the pharmacy aisle.
My mom had to choose between her insulin and her rent last year. She didn’t tell me until she ended up in the ER. And now they want us to be ‘grateful’ because they’re ‘investing in domestic production’? Like, what? After they made billions during the pandemic?
And don’t even get me started on how they let people hoard inhalers like toilet paper. That’s not ‘panic buying’-that’s survival. And the system rewards hoarders and punishes the sick.
Someone needs to start a protest. Like, outside the FDA. With signs. And chants. And maybe a giant inflatable insulin syringe.
I’m done being polite.
Kunal Majumder
January 14, 2026 AT 06:20Hey, I’m from India and I’ve worked in pharma logistics. The truth? We make most of the world’s generics, but we’re not paid enough to keep up. When energy prices spike in Europe, the cost of our raw materials jumps-and we can’t raise prices because U.S. buyers demand the lowest bid. So we cut corners. Or stop making it.
But here’s the good part: things are changing. More Indian companies are opening U.S. offices. More are getting FDA-approved for dual sourcing. It’s slow, but it’s happening.
And if you’re struggling with meds? Talk to your pharmacist. They know the back channels. I’ve seen them get people stuff no one else could. You’re not alone. Keep asking. Keep pushing. You’ve got this.
Aurora Memo
January 15, 2026 AT 15:08This post resonated deeply. I’ve seen patients delay medications because they’re afraid of the cost, or because they don’t know where to turn. The fear is real. The silence is louder.
I work with community health centers, and I’ve learned that the most powerful tool isn’t policy-it’s connection. A pharmacist who remembers your name. A nurse who helps you fill out the assistance form. A friend who shares their extra pills.
Small acts matter. They save lives.
If you’re reading this and you’re okay-please, reach out to someone who isn’t. A text. A call. A ride to the pharmacy. You don’t need to fix the system. Just be there.
chandra tan
January 16, 2026 AT 16:09Back home in India, we call this ‘pharma roulette’. You never know if your medicine will be there. Sometimes you wait weeks. Sometimes you pay double. Sometimes you just don’t take it.
But here’s the thing-we’ve learned to adapt. We trade meds with neighbors. We use Ayurvedic backups when we can. We ask the pharmacist: ‘Is there another brand?’
It’s not ideal. But it’s survival. And honestly? I think Americans are learning the same lessons now. Maybe that’s the silver lining-we’re all just trying to stay alive.
And hey-if you ever come to India, I’ll show you where to find the good stuff. 😊
Dwayne Dickson
January 16, 2026 AT 20:10Let’s deconstruct the narrative: the claim that ‘supply chains stabilized’ is statistically misleading. The Global Supply Chain Pressure Index measures transport delays and port congestion-but it does not account for production capacity, labor strikes, or regulatory bottlenecks. The real metric-pharmaceutical output per capita-has not recovered.
Furthermore, the Inflation Reduction Act’s domestic API funding is allocated through a competitive grant process that favors established firms with lobbying power. Small manufacturers are excluded. This isn’t resilience-it’s consolidation under the guise of reform.
And the suggestion that ‘mail-order pharmacies’ solve the problem ignores the digital divide. Many elderly, low-income, and rural patients lack reliable internet, transportation, or the literacy to navigate complex portals. This is equity theater.
The system is not broken. It was designed this way.
Ted Conerly
January 16, 2026 AT 22:40I’ve been in this game for 20 years. I’ve seen shortages come and go. But this one? It’s different.
What’s changed isn’t the supply-it’s the mindset. Patients are finally speaking up. Pharmacists are sharing inventory. Doctors are prescribing alternatives. And companies? They’re starting to listen.
Yes, prices are still high. Yes, some meds are still missing. But the system is waking up.
Don’t give up. Keep asking. Keep advocating. And if you’re lucky enough to have access? Help someone who doesn’t.
That’s how real change happens.
Ian Cheung
January 17, 2026 AT 11:27My dad’s blood pressure med disappeared for six months. We found it at a pharmacy in Nebraska. He drove 300 miles for it. No one talked about it. No one made a movie. We just did what we had to do.
Healthcare isn’t a market. It’s a heartbeat.
And someone’s always gonna be left behind.
McCarthy Halverson
January 17, 2026 AT 14:19Start refilling early. Ask for alternatives. Use the FDA list. Patient programs exist. You’re not helpless.
Do it.
lisa Bajram
January 19, 2026 AT 07:56Wait-so you’re telling me that after all this, the real solution is just… asking nicely? And checking a website? And hoping someone else has extra pills?
That’s it? That’s the entire plan?
I’m sorry, but that’s not a system. That’s a survival guide for a dystopian novel.
And now I’m crying again. Not because I’m weak. Because I’m tired.