Managing Skin Reactions from Topical Fluorouracil: Tips & Treatments

Fluorouracil Skin Reaction Assessment Tool
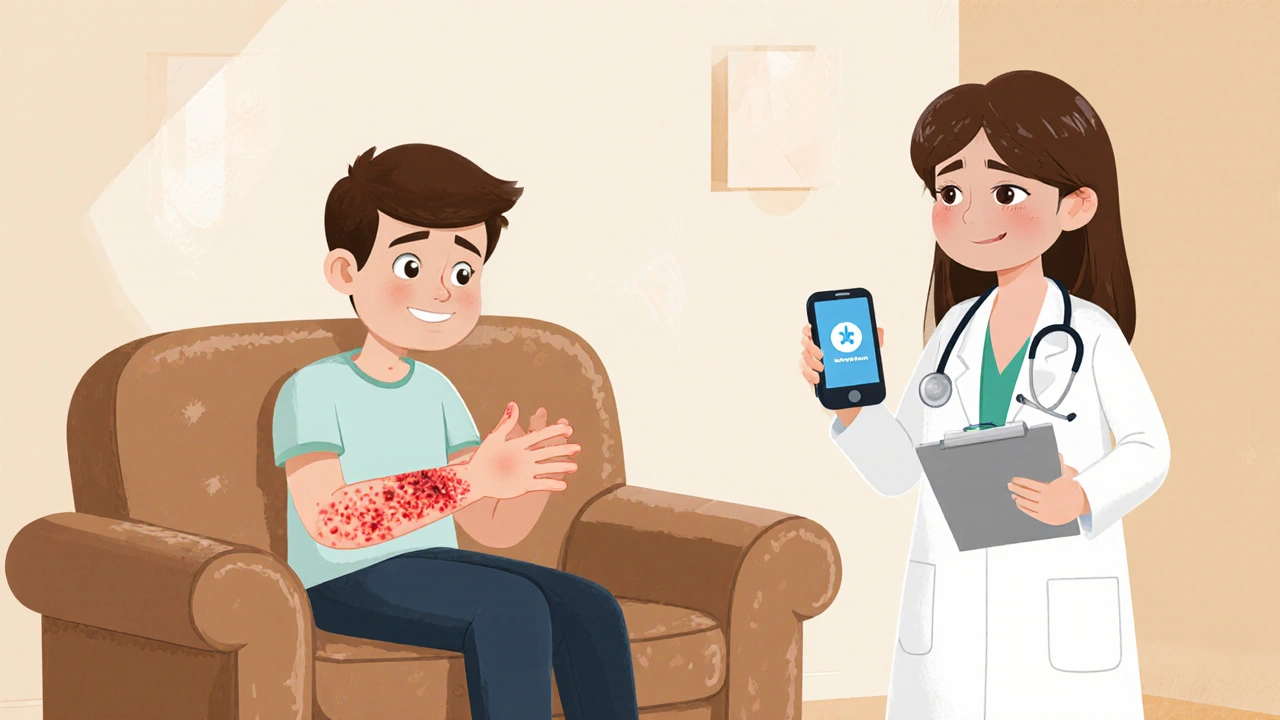
Assess Your Skin Reaction
Select the symptoms you're experiencing to determine reaction severity and get appropriate guidance.
Recommended Actions
When to Seek Medical Help
Dealing with topical fluorouracil skin reactions can feel overwhelming, but a clear plan makes it manageable. Whether you’re treating actinic keratoses or a superficial skin cancer, the cream’s powerful effect often comes with redness, peeling, or itching. This guide walks you through how to recognize, soothe, and when to seek professional help.
What is Topical Fluorouracil?
When you apply Topical Fluorouracil is a chemotherapy cream used to treat actinic keratoses and superficial skin cancers, you’re using a medication that interferes with DNA synthesis in abnormal skin cells. It’s most commonly prescribed for Actinic Keratosis is a precancerous lesion caused by long‑term sun exposure and for early‑stage basal or squamous cell carcinoma. Because it targets rapidly dividing cells, the surrounding healthy skin can react, leading to the irritation many users notice.
Why Do Skin Reactions Occur?
The skin’s response stems from two main mechanisms. First, the drug’s cytotoxic action creates an Irritant Contact Dermatitis is an inflammation caused by direct chemical irritation that feels like burning or stinging. Second, a smaller percentage of patients develop an Allergic Contact Dermatitis is an immune‑mediated reaction that can cause swelling, itching, and spreading redness. Knowing which type you’re experiencing helps guide the right soothing strategy.
Assessing Severity: Know the Signs
Before you jump into treatment, pause and evaluate how bad the reaction is. Look for these clues:
- Mild: Light redness, occasional peeling, minimal discomfort.
- Moderate: Intense redness, noticeable swelling, itching that interrupts daily activities.
- Severe: Large areas of blistering, severe pain, fever, or signs of infection such as pus.
If you spot any severe signs, it’s time to call a Dermatologist is a skin specialist trained to diagnose and treat complex skin conditions right away.
Step‑by‑Step Home Care for Mild to Moderate Reactions
Most skin reactions can be calmed at home with a structured routine. Follow these six steps:
- Patch Test is a simple method where a small amount of cream is applied to a limited skin area to gauge tolerance. Do this before each new treatment cycle.
- Wash the treated area gently with lukewarm water and a mild, fragrance‑free cleanser. Pat dry-don’t rub.
- Apply a fragrance‑free Moisturizer is a skin‑hydrating product that restores barrier function while the skin heals.
- For persistent redness, use a thin layer of over‑the‑counter Hydrocortisone is a low‑strength steroid cream that reduces inflammation. Limit use to 7‑10 days.
- Apply a Cold Compress is a cool, damp cloth that eases burning and swelling for 10‑15 minutes, several times a day.
- Finish with broad‑spectrum Sun Protection is essential; use a physical sunscreen SPF 30+ and wear protective clothing whenever outdoors.
Detailed Guidance for Each Home‑Care Step
Patch Test: Apply a pea‑sized dab on your inner forearm. Wait 24‑48 hours. If no worsening occurs, you’re likely safe to continue full‑area treatment.
Gentle Cleansing: Avoid harsh soaps, alcohol‑based wipes, or exfoliating scrubs. They can strip the skin’s natural oils and worsen irritation.
Moisturizing: Look for products with ceramides, hyaluronic acid, or colloidal oatmeal. Apply while the skin is still slightly damp to lock in moisture.
Hydrocortisone Use: One thin layer, twice daily, works best. Do NOT combine with other strong steroids unless a doctor advises.
Cold Compress: Use a clean washcloth soaked in cool water, wring out excess, and press gently on the affected zone. Never apply ice directly to the skin.
Sun Protection: Reapply sunscreen every two hours, especially after sweating or washing. Hats, long sleeves, and UV‑blocking sunglasses add extra defense.

When to Seek Professional Help
If any of the following occur, schedule an appointment promptly:
- Blistering or oozing that spreads beyond the treatment area.
- Severe pain unrelieved by over‑the‑counter measures.
- Fever, chills, or swollen lymph nodes.
- Reaction that worsens after 7‑10 days despite home care.
A Dermatologist can assess whether the reaction is allergic, irritant, or a sign of infection and may prescribe prescription‑strength steroids or adjust your fluorouracil regimen.
Medication Adjustments: Talk to Your Prescriber
Sometimes the best move is to tweak the fluorouracil schedule. Your doctor might suggest:
- Reducing application frequency (e.g., every other day instead of daily).
- Shortening the treatment course by a few days.
- Temporarily pausing the medication until the skin recovers.
Never stop the cream abruptly without medical guidance, as incomplete treatment can leave precancerous lesions untreated.
Adjunctive Relief Options
For pain or especially stubborn irritation, consider these adjuncts:
- Lidocaine is a topical anesthetic that numbs the skin for temporary relief. Apply a thin layer before bedtime.
- Healing ointments containing panthenol or petrolatum create a protective barrier and support tissue repair.
- Oral antihistamines (e.g., cetirizine) can diminish itching if an allergic component is suspected.
Lifestyle Tips to Support Healing
Beyond direct skin care, some habits speed recovery:
- Avoid hot showers, saunas, and steam rooms while the area is inflamed.
- Wear soft, breathable fabrics-cotton is best.
- Stay hydrated; good internal moisture helps skin regenerate.
- Limit alcohol and smoking, as both impair wound healing.
Tracking Progress: What to Monitor
Keep a simple journal or photo log. Note the date you start the cream, any new symptoms, and how each home‑care step affects the skin. Most reactions peak around day 5‑7 and gradually improve by day 14. If improvement stalls after three weeks, reach out to your prescriber.
Quick Comparison: Managing Reactions by Severity
| Severity | Typical Symptoms | Home‑care Actions | When to Call a Doctor |
|---|---|---|---|
| Mild | Light redness, mild peeling | Gentle cleansing, moisturizer, sun protection | Rare - only if symptoms persist >10 days |
| Moderate | Intense redness, itching, swelling | Patch test, hydrocortisone, cold compress, moisturizer | Seek dermatologist if swelling spreads or pain worsens |
| Severe | Blisters, oozing, fever, widespread pain | Stop application, keep area clean, cool compress | Immediate medical evaluation - possible infection or allergic reaction |
Wrapping Up
Skin reactions to Topical Fluorouracil are common, but they’re manageable with the right steps. Start with a gentle routine, stay alert to warning signs, and keep open communication with your dermatologist or prescribing clinician. With patience and proper care, you’ll clear the precancerous lesions while keeping your skin comfortable.
Frequently Asked Questions
How long should I wait before seeing improvement?
Most patients notice the redness peaking around days 5‑7 and a gradual fade by day 14. If no improvement occurs after three weeks, contact your prescriber.
Can I use a stronger steroid cream instead of hydrocortisone?
Only under a dermatologist’s direction. Stronger steroids carry higher risks of skin thinning and should be reserved for severe allergic reactions.
Is it safe to apply sunscreen on the treated area?
Yes, and it’s crucial. Use a physical sunscreen (zinc oxide or titanium dioxide) and reapply every two hours to protect the healing skin from UV‑induced damage.
What if I develop a rash on a different part of my body?
That may signal a systemic allergic response. Stop using the cream and seek immediate medical advice.
Can I continue using the cream while on a moisturizer?
Apply the moisturizer after the fluorouracil has fully absorbed (usually 15‑20 minutes). This helps keep the barrier intact without diluting the medication.






alex montana
October 18, 2025 AT 19:53Wow!!! The moment you slap that Fluorouracil on, it feels like a wildfire on your skin!!! The burning, the peeling… I can almost hear the skin screaming!!! It's not just a rash; it's a battle!!!
Wyatt Schwindt
October 31, 2025 AT 21:33I get that the itching can be really uncomfortable, so stick to the gentle cleanser and moisturizer and you should see improvement within a week.
Fabian Märkl
November 14, 2025 AT 00:13Hey folks! 🙌 Keep that routine tight-wash, moisturize, and slap on a cool compress when it burns. Your skin will thank you and you’ll stay on track to clear those lesions! 🌟💪
Natala Storczyk
November 27, 2025 AT 02:53THIS ISN'T SOME FOREIGN MALADY-IT'S YOUR OWN BODY REACTING TO A POWERFUL TREATMENT!!! DON'T LET A LITTLE REDNESS STOP YOU FROM PROTECTING OUR NATION'S HEALTH!!! PUSH THROUGH WITH STRONG STEROIDS ONLY IF YOUR DOCTOR SAYS SO!!!
Karla Johnson
December 10, 2025 AT 05:33When you first notice the tingling sensation after applying fluorouracil, it’s important to pause and document the exact time and location of the reaction. A thorough journal not only helps you track the progression but also provides valuable data for your dermatologist to assess the severity. Begin by performing a patch test on a discreet area of skin, such as the inner forearm, and wait a full 48 hours before interpreting the result. If the test area remains free of new erythema or blistering, you can be reasonably confident that the larger treatment zone will not experience an acute hypersensitivity reaction. However, if you observe escalating redness, swelling, or a rash that spreads beyond the test site, discontinue the cream immediately and seek medical advice. In the meantime, gentle cleansing with a fragrance‑free, non‑soap cleanser protects the skin barrier without stripping natural oils. Follow the wash with a moisturizer rich in ceramides and hyaluronic acid while the skin is still slightly damp to lock in hydration. For persistent inflammation, a thin layer of low‑strength hydrocortisone applied twice daily can calm the immune response, but it should not exceed ten days without professional guidance. Cold compresses-using a clean, cool, damp washcloth for ten to fifteen minutes several times a day-provide rapid relief from burning and reduce edema. Avoid hot showers, saunas, or vigorous rubbing, as heat can exacerbate vasodilation and intensify the sensation of itchiness. Sun protection is non‑negotiable; a mineral sunscreen with zinc oxide applied liberally and reapplied every two hours shields the healing tissue from UV‑induced DNA damage. If you notice any signs of infection such as purulent discharge, increasing pain, or fever, treat it as an emergency and contact a healthcare provider without delay. Sometimes clinicians will adjust the fluorouracil regimen, reducing frequency to every other day or shortening the overall course, which can dramatically lessen adverse effects while maintaining efficacy. Oral antihistamines like cetirizine may be useful if you suspect an allergic component, but they are adjuncts rather than primary treatments. Remember that the peak of the reaction typically occurs around days five to seven, after which a gradual improvement should become evident if the home‑care plan is followed diligently. Staying hydrated, maintaining a balanced diet, and avoiding smoking further support the skin’s natural repair mechanisms and lead to a smoother recovery.
Ayla Stewart
December 23, 2025 AT 08:13That’s a solid step‑by‑step guide; I especially like the reminder about using a mineral sunscreen and keeping a symptom diary.
Liberty Moneybomb
January 5, 2026 AT 10:53Don’t be fooled by the “friendly” advice-big pharma wants you to think a simple routine is enough while they hide the long‑term skin damage behind glossy ads!!! The truth is out there, and you need to stay vigilant!!!
Alex Lineses
January 18, 2026 AT 13:33From a dermatologic pharmacokinetic perspective, maintaining optimal stratum corneum hydration facilitates proper drug penetration while minimizing inflammatory cytokine release; therefore, integrate occlusive barrier enhancers post‑application to modulate the percutaneous absorption curve.
Bethany Torkelson
January 31, 2026 AT 16:13Stop spouting that fancy jargon and actually tell us what to put on the skin-enough with the lab speak!!!
Grace Hada
February 13, 2026 AT 18:53Skin pain is the universe reminding you of mortality.