Look-Alike, Sound-Alike Medication Names That Cause Errors: Real Risks and How to Stop Them

Every year, people get the wrong medicine-not because of a mistake in the prescription, but because two drugs look or sound too much alike. This isn’t rare. One in four medication errors in U.S. hospitals comes from this exact problem. And it’s not just a paperwork glitch. These mix-ups can kill.
What Exactly Are Look-Alike, Sound-Alike (LASA) Drugs?
Look-alike, sound-alike (LASA) drugs are medications that are confusing because of how they’re written, spoken, packaged, or even shaped. It’s not about being identical-it’s about being close enough to trick someone under pressure. Take HYDROmorphone and hYDROcodone. Both are powerful painkillers. But one is for severe pain in hospitals. The other is for mild to moderate pain at home. If a nurse hears "hydro" in a busy ER, they might grab the wrong vial. That’s not a theory-it’s happened. The FDA started using tall man lettering (capitalizing the different parts) to help: HYDROmorphone vs. hYDROcodone. But even that doesn’t always work. Then there’s simvastatin 10 mg and simvastatin 20 mg. Same drug. Different strength. But when a pharmacist is rushing between 20 prescriptions, they might grab the wrong bottle. That’s not a typo-it’s a dosing error that can cause muscle damage or liver failure. And it’s not just pills. Vecuronium (a muscle relaxant) and Versed (a sedative) look nothing alike on paper-but in a dim ICU room, with a tired nurse and a muffled voice over the intercom, the names blur. One patient nearly died because of this mix-up. The nurse caught it at the last second.Why Do These Errors Keep Happening?
You’d think hospitals would have fixed this by now. But the truth is, the system is still set up to make these mistakes easy. First, human factors play a huge role. Nurses and pharmacists aren’t careless-they’re overwhelmed. During shift changes, night shifts, or when understaffed, the brain takes shortcuts. A name like "levoTHYroxine" and "SYNTHROID" both mean thyroid meds. If someone says "give me the thyroid pill," the wrong one gets pulled. Second, packaging is often identical. Two different drugs in similar bottles, same color, same font size. Even the label layout is the same. One study found that 25% of LASA errors came from packaging confusion-not the name itself. Third, new drugs keep getting approved with names that are too similar to existing ones. In 2022, the FDA rejected 34 new drug names because they were too close to existing ones. That’s up from 22 in 2018. But many still slip through. Melphalan and meloxicam were added to the high-risk list in early 2024. One’s a chemo drug. The other’s a pain reliever. Say them out loud. They’re nearly identical.The Most Dangerous LASA Pairs
Some mix-ups are more deadly than others. Here are the most dangerous pairs still in use:- Doxorubicin and Daunorubicin - both chemotherapy drugs. Give the wrong one, and you can cause heart failure.
- Insulin glargine and Insulin lispro - one is long-acting, the other fast-acting. Mixing them can send a diabetic into a coma.
- Clonidine and Clonazepam - one lowers blood pressure, the other treats seizures. Confusing them can cause dangerous drops in BP or seizures.
- Naltrexone and Naloxone - one blocks opioids long-term for addiction. The other reverses overdoses. Give naltrexone during an overdose? The person dies.
- Cisplatin and Carboplatin - both chemo drugs. Different dosing, different side effects. Wrong one? Kidney damage or bone marrow failure.

What’s Being Done to Fix This?
There are tools. But not everyone uses them well. Tall man lettering (like HYDROmorphone) is the most common fix. It’s been around since 2001. But studies show it only works if people know why it’s there. If you don’t know that the capital letters are a warning, you just see weird spelling. One review called it a "quasi-placebo effect." It helps-but it’s not enough. Electronic health records (EHRs) like Epic and Cerner now have built-in LASA alerts. Epic’s "SafeMed" module cut name-confusion errors by nearly 30% in a 12-hospital trial. But smaller clinics? Many still use paper lists or outdated software. Only 38% of small hospitals have full LASA protocols. Big ones? 72% do. Training is required-usually 2 to 4 hours a year. But in oncology or ICU units, staff need quarterly refreshers. Many places skip this. Why? Time. Budget. Burnout. The Joint Commission says every hospital should make its own LASA list-not copy one from another hospital. That’s smart. A small clinic doesn’t use chemotherapy. Why waste time warning about drugs they never handle? But only half of hospitals actually do this properly.What Can You Do as a Patient?
You’re not powerless. Here’s how to protect yourself:- Ask for the generic name. If your doctor says "give me the thyroid pill," ask: "Is that levothyroxine or Synthroid?"
- Check the label. When you get a prescription, look at the name, strength, and color. Does it match what you’ve taken before? If not, ask.
- Speak up during handoffs. If you’re in the hospital, ask nurses to say the full name of each drug before giving it. "Is this hydromorphone or hydrocodone?"
- Know your high-risk meds. If you’re on insulin, blood thinners, or chemo, be extra careful. These are the drugs most often mixed up.
- Use one pharmacy. If you get prescriptions from multiple places, the risk goes up. One pharmacy can track all your meds and flag conflicts.
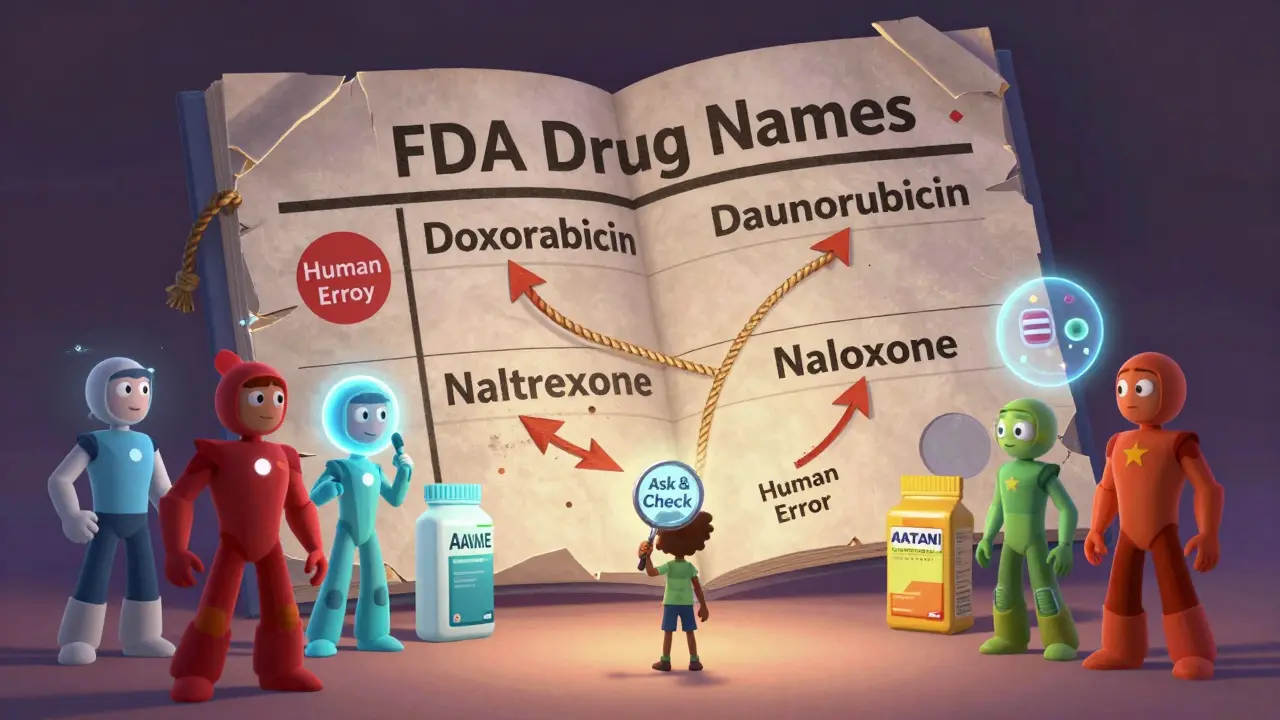
The Bigger Picture: Why This Isn’t Just a "Human Error" Problem
The biggest myth is that LASA errors are caused by "careless staff." They’re not. They’re caused by a system that lets dangerous names get approved, uses similar packaging, and doesn’t consistently use safeguards. The World Health Organization says we need to design safety into the system-not just train people to avoid mistakes. That means:- Rejecting new drug names that sound too similar to existing ones
- Standardizing packaging colors and shapes across all manufacturers
- Using AI to flag verbal orders in real time (like the Johns Hopkins trial that’s 89% accurate)
- Making LASA checks mandatory in every EHR, not optional
What’s Next?
The future is starting to shift. The FDA is drafting new rules that would require all new drug names to pass a computerized similarity test before approval. That’s huge. If it passes, we might finally stop new dangerous names from entering the market. The International Pharmaceutical Federation wants global standards for drug naming by 2030. That’s ambitious-but necessary. Right now, a drug approved in the U.S. might have a name that’s dangerous in Canada or Australia. And technology is catching up. AI voice recognition systems are being tested to listen to doctors say "give me the hydromorphone" and instantly flag: "Did you mean hydrocodone?" Early results show promise. This isn’t about blaming nurses or pharmacists. It’s about fixing a broken system that puts patients at risk every single day.What are the most common look-alike, sound-alike drug pairs?
The most common dangerous pairs include hydromorphone vs. hydrocodone, insulin glargine vs. insulin lispro, doxorubicin vs. daunorubicin, clonidine vs. clonazepam, and naltrexone vs. naloxone. Even small differences in strength-like simvastatin 10 mg vs. 20 mg-can cause errors. These mix-ups happen because names look or sound too similar, especially under pressure.
How often do LASA errors happen?
About one in four medication errors in U.S. hospitals is caused by look-alike, sound-alike confusion, according to research from Medscape and the Anesthesia Patient Safety Foundation. In some settings, like oncology units, the rate is even higher-up to 92% of physicians report near-misses involving similar drug names.
Does tall man lettering actually work?
Tall man lettering (like HYDROmorphone vs. hYDROcodone) helps-but only if people understand why it’s used. Studies show it reduces errors by a small amount, but it’s not a fix on its own. If staff don’t know the purpose, they just see odd capitalization. It works best when combined with electronic alerts, training, and standardized packaging.
Can I trust my pharmacy to catch these errors?
Pharmacists are trained to catch these mistakes, but they’re often overworked. A 2022 study found that 68% of LASA errors happen during administration, often during busy shifts or handoffs. Always double-check your medication name, strength, and appearance when you pick it up. If it looks different than before, ask why.
Are there any new technologies helping prevent these errors?
Yes. AI-powered voice recognition systems are being tested to detect LASA mix-ups during verbal orders. One Johns Hopkins project achieved 89.3% accuracy. EHR systems like Epic now have built-in LASA alerts that flag similar names during prescribing. Some hospitals are also using color-coded labels and barcode scanning to reduce errors.






Glenda Marínez Granados
January 20, 2026 AT 01:42Malvina Tomja
January 20, 2026 AT 18:03Yuri Hyuga
January 22, 2026 AT 17:26MARILYN ONEILL
January 23, 2026 AT 22:12Ashok Sakra
January 24, 2026 AT 18:44Andrew Rinaldi
January 26, 2026 AT 00:50Gerard Jordan
January 27, 2026 AT 19:19michelle Brownsea
January 27, 2026 AT 20:02