How to Read Prescription Labels for Inhalers, Patches, and Injectables
Getting the right medicine is only half the battle. If you don’t know how to read the label on your inhaler, patch, or injection, you could be putting your health at risk. Unlike pills you swallow, these delivery systems have unique rules - and the labels reflect that. A 2022 study found that nearly 39% of medication errors involving these devices happened because someone misread the label. That’s not a small number. It’s a warning.
Why Inhaler Labels Are Different
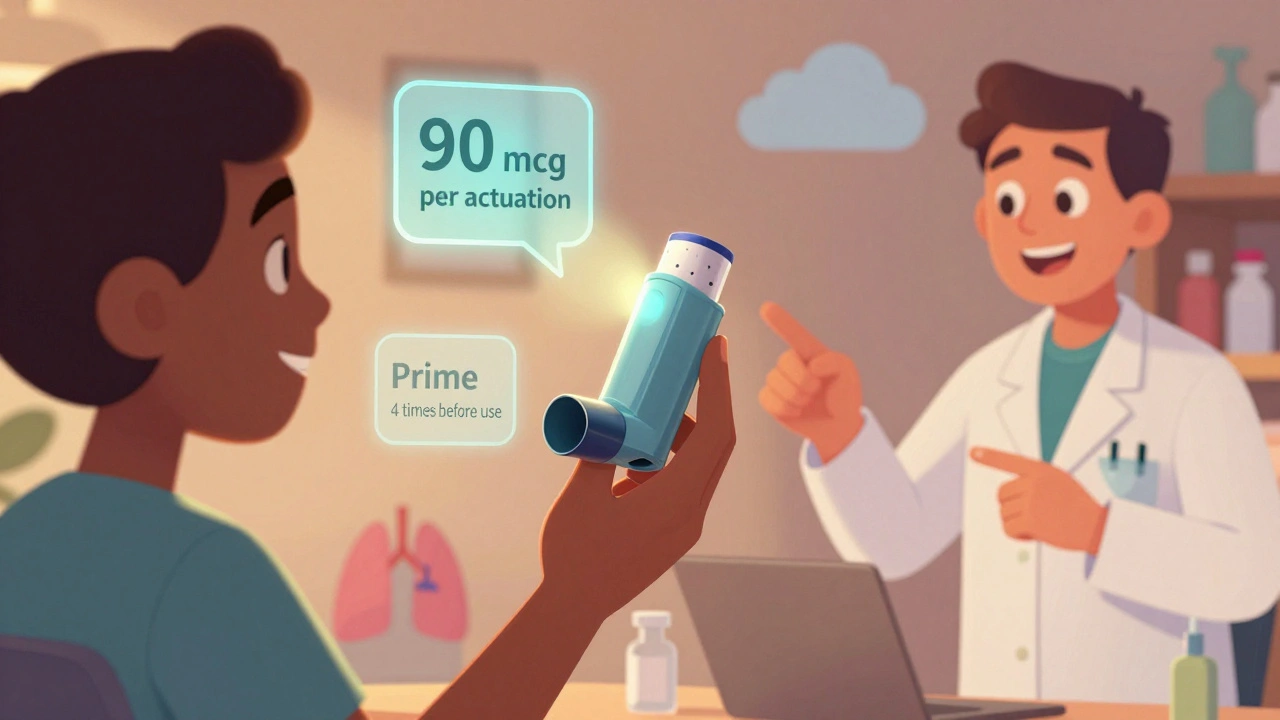
Inhalers look simple - a metal canister with a mouthpiece. But inside, it’s a precision device. The label doesn’t just say "take two puffs." It tells you exactly how much medicine each puff delivers. Look for phrases like "albuterol sulfate 90 mcg per actuation." That’s the dose. If you don’t know what that means, you might think you’re getting more than you are.Another common mistake? Thinking the inhaler is full because it still feels heavy. But after about 120 puffs, the canister might be empty even if it still sprays. That’s why modern inhalers now have built-in dose counters. Since May 2024, the FDA requires them on all new inhalers. If yours doesn’t have one, ask your pharmacist for a replacement. Don’t guess how many doses are left.
Also check for "prime before first use" instructions. Most new inhalers need 4 test sprays into the air before you use them for the first time. Skip this step, and your first dose might be useless. Shake the inhaler? Only if the label says so. Suspension inhalers need shaking. Solution inhalers don’t. Mixing that up can change how well the medicine works.
What Patch Labels Won’t Tell You Out Loud
Transdermal patches stick to your skin and slowly release medicine over hours or days. But the label doesn’t always say what you need to know. For example, a fentanyl patch labeled "25 mcg/hour" means you get 25 micrograms every hour - not 25 total. If you think it’s a 72-hour dose of 25 mcg total, you’re dangerously wrong.Placement matters too. Most patches say "apply to clean, dry skin" - but they rarely say where to put them. Fentanyl patches go on the upper back, chest, or arm. Never on a scar, burn, or irritated area. And never on skin that’s hot. Heat increases absorption. A study in 2022 found that wearing a patch while in a hot tub or sauna can boost drug levels by up to 50%. That’s enough to cause an overdose.
And here’s something no one talks about: disposal. Used fentanyl patches still hold 70-80% of their original dose. The FDA issued a safety alert in 2022 after 147 cases of accidental exposure - mostly from kids or pets finding thrown-away patches. Always fold your used patch in half with the sticky sides together, and flush it down the toilet. Or return it to your pharmacy. Never toss it in the trash.
Injectables: The Hidden Dangers in Small Print
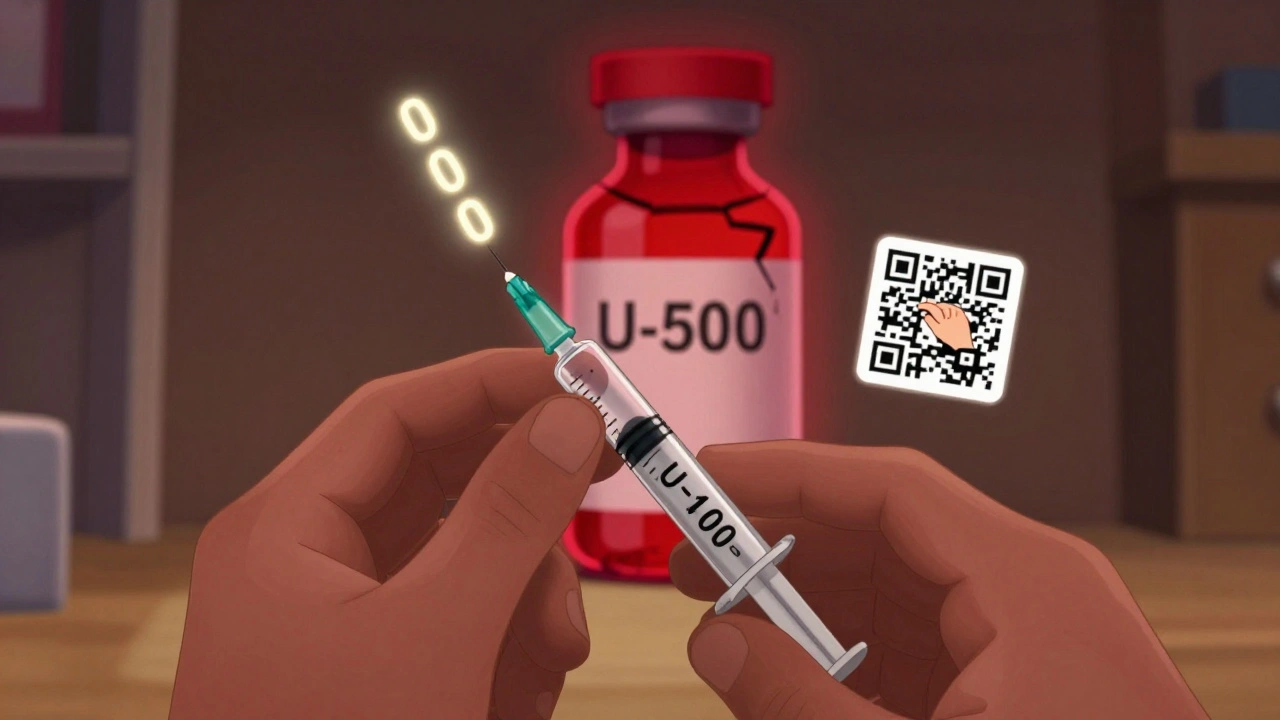
Injectables are the most dangerous if misread. Insulin is the most common example. You might see "insulin glargine 100 units/mL" on the label. That means each milliliter has 100 units. But some people read it as "100 units total" and take the whole vial. That’s a fatal mistake.There are different concentrations. U-100 is standard. But U-500 insulin is five times stronger. If you accidentally use U-500 thinking it’s U-100, you could overdose by 400%. Labels now use bold, large fonts for concentration - but you still have to look. The American Diabetes Association says 19.3% of insulin errors in 2023 came from misreading this.
Reconstitution matters too. Some injectables come as powder and need mixing with liquid. The label will say "add 1 mL sterile water" - not "add water." Use the exact amount. Too much dilutes the dose. Too little makes it too strong. Always check the expiration date after mixing. Some reconstituted medicines last only 24 hours.
Storage is another hidden rule. Some injectables need refrigeration. Others don’t. Keep them at room temperature unless the label says otherwise. And never freeze insulin - it breaks down and stops working.

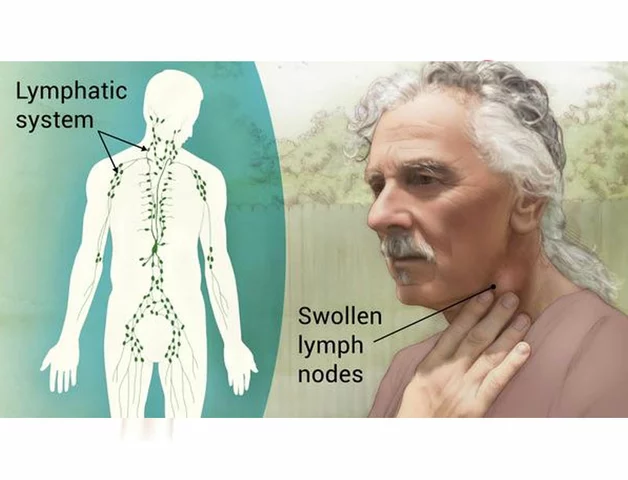
Why Auxiliary Labels Matter
You’ve probably seen those small stickers on your prescription bottle: "Do not expose to heat," "Apply to clean skin," "Shake well." These are auxiliary labels. They’re not part of the main label - but they’re just as important.As of 2023, 92% of prescriptions for inhalers, patches, and injectables come with at least one auxiliary label. These are added by the pharmacist to warn you about things the manufacturer’s label doesn’t cover. A patch might have a sticker saying "Do not cut." That’s because cutting a fentanyl patch can cause a sudden, dangerous release of the drug. One FDA analysis found cutting increases overdose risk by nearly five times.
Don’t ignore these stickers. They’re there for a reason. If you don’t understand one, ask your pharmacist to explain it. Don’t assume.
How Labels Are Changing - And How to Use the New Tools
The industry is finally catching up. Since 2021, the FDA has required standardized pictograms on new specialized delivery systems. These are simple drawings showing how to use the device - like a hand holding an inhaler, or a patch being applied to the arm. A 2023 study showed these pictograms reduced errors by 37% compared to text-only instructions.Many new labels now include QR codes. Scan it with your phone, and you’ll see a short video showing exactly how to use the device. In 2021, only 12% of these products had QR codes. By 2023, that jumped to 67%. Patient comprehension improved by 29% when people used them.
By 2026, pharmacies will start using AI tools to double-check labels before handing out medication. Pilot programs have already cut labeling errors by 41%. And by 2027, some labels will let you use your phone’s camera to see an augmented reality demo of how to use the inhaler or injectable - right over the actual device.
What to Do If You’re Still Confused
You’re not alone. A 2023 JAMA study found only 38% of patients got a full 15-20 minute explanation from their pharmacist. That’s not enough. Here’s what to do:- Always ask: "Can you show me how to use this?" Don’t just take the bottle and leave.
- Bring your inhaler, patch, or syringe to the pharmacy. Ask them to demonstrate in front of you.
- If you use multiple devices, keep a simple chart: one column for the name, one for the dose, one for how often, and one for storage. Update it every time you get a new prescription.
- Use the QR code. Watch the video. Repeat it if you need to.
- If you’re blind or have low vision, ask for a talking label or braille version. Many pharmacies offer this now.
One patient on Reddit shared that her inhaler label said "2 puffs twice daily." She thought it meant four total puffs a day - not four puffs, twice a day. That mistake nearly sent her to the ER. She’s fine now. But she didn’t learn from the label. She learned from her pharmacist.
Final Checklist Before You Use Any of These
Before you use your inhaler, patch, or injection, run through this quick list:- Is the device labeled with a dose counter? (Inhalers only)
- Does the label say how much medicine each puff, hour, or mL delivers?
- Is there a "prime" or "shake" instruction? And does it apply to this type?
- Is there a "do not cut," "do not expose to heat," or "apply to clean skin" sticker?
- Does the concentration match what your doctor prescribed? (Especially for insulin)
- Is the expiration date still good - especially if it’s been mixed or opened?
- Do I know how to dispose of this safely?
If you can’t answer any of these, don’t use it. Call your pharmacist. Go back to the pharmacy. Ask again. It’s better to be slow than sorry.
Medicine is powerful. But labels are your safety net. Treat them like instructions for a life-saving machine - because that’s exactly what they are.
What should I do if my inhaler runs out before the label says it should?
If your inhaler feels empty but the dose counter still shows doses left, it’s likely a mechanical issue. The canister may be empty even if it still sprays. Always trust the dose counter over how the inhaler feels. If the counter shows zero, stop using it - even if you can still spray. Contact your pharmacy for a refill. Never try to refill it yourself.
Can I cut my medication patch to reduce the dose?
Never cut a transdermal patch unless your doctor specifically tells you to. Cutting a patch like fentanyl can cause a sudden, dangerous release of the full dose all at once. The FDA warns that cutting increases overdose risk by nearly five times. Even if the patch looks like it’s meant to be split, it’s not safe. Ask your doctor for a lower-dose patch instead.
Why does my insulin label say U-100 and not 100 units?
"U-100" means 100 units per milliliter. It’s a standard way to show concentration. If you see U-500, that’s five times stronger. Many insulin errors happen because people think "100 units" means the total amount in the vial - not the concentration. Always read "U-100" as "100 units per mL." Never assume. Double-check with your pharmacist if you’re unsure.
What if I accidentally use the wrong device - like an inhaler instead of a patch?
If you accidentally use the wrong delivery system, call your pharmacist or doctor immediately. Inhalers are designed for lungs, patches for skin absorption, and injectables for direct blood delivery. Using them wrong can lead to overdose or underdose. For example, inhaling a patch medication could cause severe lung irritation. Never guess. Get help right away.
Are QR codes on medication labels safe to scan?
Yes. QR codes on prescription labels are provided by the manufacturer and link directly to official video instructions hosted on secure, verified websites. They’re designed to help you use your medicine safely. Scan them with your phone’s camera or a free QR reader app. Don’t worry about malware - these are regulated and monitored by the FDA and pharmacy boards. If the link looks suspicious, call your pharmacy to confirm.





Mark Curry
December 5, 2025 AT 23:39Just read this and it hit me - we treat meds like they’re magic boxes. But they’re machines. Tiny, life-or-death machines. And labels? They’re the manuals. No one reads manuals anymore. We just press buttons and hope. This post is the wake-up call we all needed.
Still, I’m glad they’re adding QR codes and pictograms. A picture’s worth a thousand words when you’re scared and tired.
And yeah - if you don’t know what U-100 means, ask. No shame in that.
Mellissa Landrum
December 7, 2025 AT 18:51so the fda just now made inhalers have dose counters??? after how many people died?? i swear these corporations wait until someone’s kid overdoses on a patch before they do ANYTHING. and now they’re gonna put qr codes on everything? like we’re all supposed to be tech wizards now? what about the elderly? what about people without smartphones? this is just more corporate theater. they don’t care - they just want to cover their butts.
aditya dixit
December 8, 2025 AT 14:19Thank you for writing this. I’ve been a pharmacist for 17 years and I’ve seen too many people skip the auxiliary labels. That little "Do not cut" sticker? It’s saved lives. I wish more patients knew how much we worry about them when they leave the counter. You’re not just a prescription number. You’re someone’s parent, sibling, friend.
And yes - if you’re confused, come back. We don’t mind. Really.
luke newton
December 8, 2025 AT 21:31people are dumb. like seriously. how do you not know that cutting a patch is suicide? i mean, it’s right there on the label. you don’t need a degree to read. you just need to not be an idiot. and now we’re gonna give people qr codes and videos? like we’re babysitting adults? this is why america’s healthcare costs are insane. people refuse to take responsibility for their own bodies. wake up.
an mo
December 9, 2025 AT 00:18Let’s quantify this: 39% of inhaler errors stem from label misinterpretation. That’s not anecdotal - that’s epidemiological. And with transdermal patches, the pharmacokinetic variance under thermal stress is non-linear - heat increases dermal permeability exponentially, not linearly. So a 50% increase in absorption? That’s a 200%+ spike in Cmax. That’s not a side effect - that’s a pharmacological cascade.
And don’t get me started on U-500 insulin. That’s not a typo. That’s a death sentence for the uneducated. The ADA’s 19.3% error rate? That’s a systemic failure of patient education infrastructure. We need mandatory pharmacist-led demonstrations - no exceptions.
Juliet Morgan
December 10, 2025 AT 19:29i used to think i was fine until my grandma almost died because she thought the patch was "one time use" and put on three at once. i didn’t know any better either. now i keep a little notebook. name, dose, how to use, where to stick it. i even took a pic of the qr code so i can watch it again. it’s not embarrassing to need help. it’s smart.
Mark Ziegenbein
December 12, 2025 AT 12:15Let me tell you something - the real tragedy here isn’t the label, it’s the erosion of human dignity in healthcare. We’ve reduced the sacred act of healing to a transactional checklist - scan the QR, tap the app, follow the video. Where’s the connection? Where’s the compassion? Where’s the pharmacist who looks you in the eye and says, "I know this is scary, let me show you again"? We’ve outsourced empathy to algorithms and now we’re surprised people are confused. This isn’t a medication issue - it’s a soul issue.
Deborah Jacobs
December 13, 2025 AT 07:52my dad’s insulin pen had a sticker that said "refrigerate after opening" - he left it on the counter for three weeks. one day he felt weird, went to the hospital - turned out the insulin was dead. no more bubbles, no more punch. just… nothing. he’s fine now but i cried for an hour. i wish someone had told him that cold doesn’t mean "bad" - it means "alive."
Also - never trust the spray sound. My inhaler made noise even when it was empty. I thought I was fine. I wasn’t.
Kylee Gregory
December 13, 2025 AT 09:27I think the most beautiful part of this is how the industry is slowly, quietly fixing itself. QR codes. Pictograms. Dose counters. These aren’t flashy marketing moves - they’re quiet acts of care. We’ve spent decades blaming patients for not understanding. But what if the problem wasn’t them? What if it was the system? Maybe we’re finally learning to speak their language - not just the language of medicine, but the language of fear, confusion, and exhaustion.
Let’s keep going.
James Moore
December 14, 2025 AT 13:31And yet - we still live in a society where a man can buy a gun with zero training, but if you need to use an inhaler, you’re expected to decode medical jargon like a PhD candidate - all while terrified, in pain, and possibly on 17 other meds. This isn’t a failure of intelligence - it’s a failure of equity. The label is a privilege. Not everyone has the time, the education, the language, or the mental bandwidth to parse "90 mcg per actuation" while their lungs are shutting down. The system should adapt to the human - not the other way around.
Philip Kristy Wijaya
December 15, 2025 AT 23:05Are you people seriously celebrating QR codes as progress? This is the same logic that told us "apps will fix everything" - then we got data breaches, privacy violations, and elderly people crying because their phone won’t scan the code. The FDA doesn’t care about you. They care about liability. They’ll slap a QR code on a patch and call it innovation while the real problem - the lack of universal healthcare, the profit-driven pricing, the pill mills - continues unchecked. This is a Band-Aid on a hemorrhage. And you’re clapping?
Manish Shankar
December 17, 2025 AT 07:38With profound respect for the author’s meticulous attention to detail, I must express my deepest appreciation for this comprehensive exposition on the critical importance of proper medication label interpretation. In my professional capacity as a healthcare provider in India, I have witnessed similar challenges among patients who, due to linguistic, educational, or socioeconomic barriers, are unable to fully comprehend the nuances of their prescribed therapies. The introduction of standardized pictograms and QR-based instructional media represents a commendable stride toward inclusive healthcare. I humbly suggest that future iterations of such labeling systems incorporate multilingual audio instructions and tactile braille elements to ensure accessibility for all. Thank you for illuminating this vital domain with such clarity and compassion.