Osteoporosis: what to know and what to do now
Osteoporosis weakens bones so they break more easily. You might not feel anything until a fall or a small bump causes a fracture. That’s why the focus is on spotting risk early, protecting bones, and lowering your chance of a break.
Who should be checked and how
If you’re a woman over 65 or a man over 70, ask your doctor about a DEXA (bone density) scan. Younger people need testing if they have risk factors: long steroid use, low body weight, early menopause, smoking, heavy alcohol, or certain medical conditions (like rheumatoid arthritis). A DEXA gives a T-score: above -1 is normal, -1 to -2.5 is low bone mass (osteopenia), and -2.5 or lower means osteoporosis.
Also check fall risk at home — poor balance, loose rugs, dim lighting, or medicines that make you dizzy raise chances of a fracture. Fixing these is often the fastest way to lower risk.
Actions that actually help
Move your body. Weight-bearing exercise (walking, stair climbing) and resistance training (bands, light weights) stimulate bone. Aim for at least 150 minutes a week of moderate activity plus two strength sessions. If balance is a problem, try tai chi or supervised physical therapy.
Get enough calcium and vitamin D. Most adults need about 1,000–1,200 mg of calcium daily from food and, if needed, supplements. Vitamin D helps your body use calcium; common targets are 800–1,000 IU daily, but check a 25(OH)D blood level — many clinicians aim for 20–30 ng/mL or higher for people at risk. Talk with your clinician before starting supplements, especially if you take other meds.
Fix habits that harm bone. Stop smoking and limit alcohol to no more than one drink a day for women and two for men. Review your medications with a doctor; some drugs (long-term steroids, some anticonvulsants) lower bone density and may need alternatives or protective therapy.
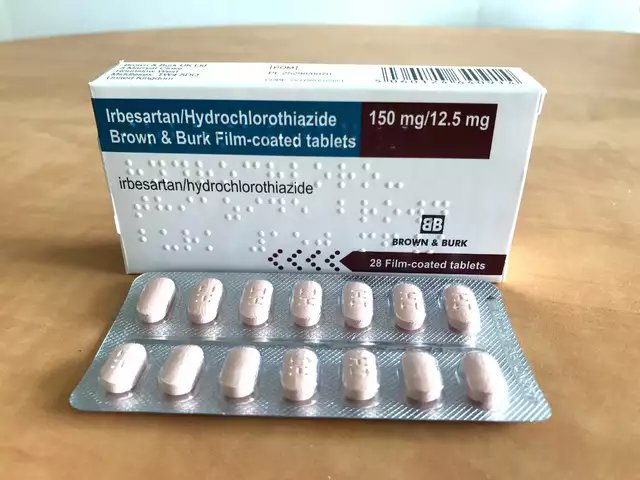
If your DEXA score or fracture risk is high, medications can cut fracture risk. Common options include bisphosphonates (alendronate, risedronate), denosumab, and anabolic agents (like teriparatide) for severe cases. Each has pros and cons — duration limits, side effects, and monitoring needs — so decisions are individual. Your doctor can run a fracture-risk calculation (FRAX) to guide choices.
Preventing fractures is more than pills. Home safety, vision checks, proper footwear, and treating balance problems matter. If you fall once, get assessed — one fall raises the chance of future falls and fractures.
Want a quick checklist to bring to your doctor? Ask: should I get a DEXA scan, what’s my fracture risk score, do I need calcium or vitamin D testing, and is medication right for me? That makes the visit focused and useful.
Small changes add up: stronger muscles, safer spaces, and the right nutrients reduce fracture risk and keep you independent. Start with one change this week — a 20-minute walk, remove a loose rug, or call to schedule a DEXA.

Fosamax for Osteoporosis: Benefits, Side Effects, and Patient Tips
Fosamax, also known as alendronate, is a popular medication for treating osteoporosis and bone loss. This article explains in plain language how Fosamax works, explores its proven benefits and side effects, and offers practical user tips. You'll learn what to expect when starting treatment, what real studies say, and how to manage risks for better bone health.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)