Mucus: Causes, When to Worry, and Simple Ways to Clear It
Mucus is sticky, annoying, and often a sign your body is working to protect you. You’ll notice more of it with colds, allergies, sinus infections, acid reflux, or when you breathe smoke and pollutants. Most of the time you can manage mucus at home. Below are clear, useful tips that actually help and quick signs that mean you should see a clinician.
What makes mucus increase and what the color means
Viruses (common cold, flu) and allergies are the top causes of extra mucus. Bacterial sinus infections may follow and tend to produce thicker, yellow or green discharge plus facial pressure. Clear mucus can be normal or allergy-related. Blood in mucus, severe shortness of breath, high fever, or symptoms that last more than three weeks deserve urgent attention. Color helps guide, but it’s not a diagnosis: colored mucus suggests an immune response, not always a bacterial infection.
Think about triggers: do your symptoms get worse around pets, pollen, or specific workplaces? Do you smoke or inhale fumes? Acid reflux can cause constant throat clearing and post-nasal drip even without nasal congestion. Noticing patterns helps your provider treat the real cause, not just the symptom.
Practical, safe ways to reduce mucus at home
Hydrate. Plain water thins mucus and makes it easier to clear. Aim for steady intake across the day rather than gulping. Warm beverages like broth or herbal tea loosen phlegm and calm the throat.
Steam and humidity. A hot shower or 10 minutes leaning over a bowl of hot water with a towel helps loosen nasal and chest mucus. Use a humidifier at night set to 30–50% if your home is dry.
Saline rinses. A saline nasal spray or rinse (neti pot or squeeze bottle) flushes out mucus and allergens. Use sterile or boiled-and-cooled water and follow package directions—twice daily when congested usually does the trick.
Over-the-counter options. Guaifenesin can help loosen chest mucus; follow label directions. Short-term oral decongestants reduce nasal swelling but avoid them if you have high blood pressure unless your doctor okays it. Nasal steroid sprays are safe long-term for allergy-related mucus and cut down post-nasal drip.
Simple habits: sleep with your head slightly elevated, use a warm compress over sinuses for comfort, avoid smoke and strong odors, and treat acid reflux by avoiding late meals and spicy foods if reflux seems linked to throat mucus.
When to see a doctor: symptoms lasting over 10–14 days, worsening after initial improvement, severe facial pain, blood in mucus, breathing trouble, or fever above 38.5°C (101.3°F). For chronic daily mucus or constant throat clearing you may need allergy testing, a sinus CT, or referral to ENT for targeted care.
If you want more detail, check related reads on infections, sinus care, and safe medication choices in our articles about bacterial invasion, antiviral treatments, and antibiotic alternatives.
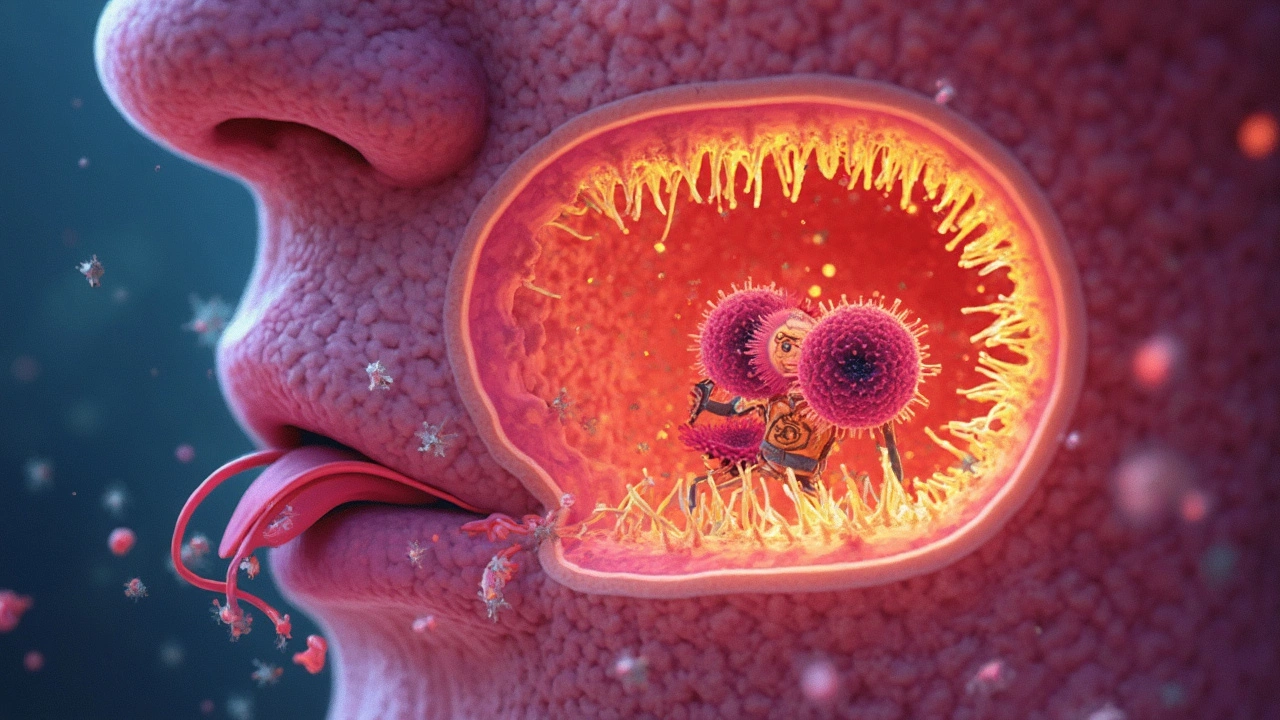
How Pharyngeal Mucous Membranes Guard Against Infection
Think of your pharyngeal mucous membranes as a security team for your throat. They trap and sweep away harmful germs before they sneak into your body. The sticky mucus, cells, and chemicals work together 24/7 to keep you safe. This article breaks down how these membranes do their job, why it matters, and what you can do to keep your throat defenses strong. You'll also get practical tips for daily habits to protect your throat.
Categories
- Medications (69)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)