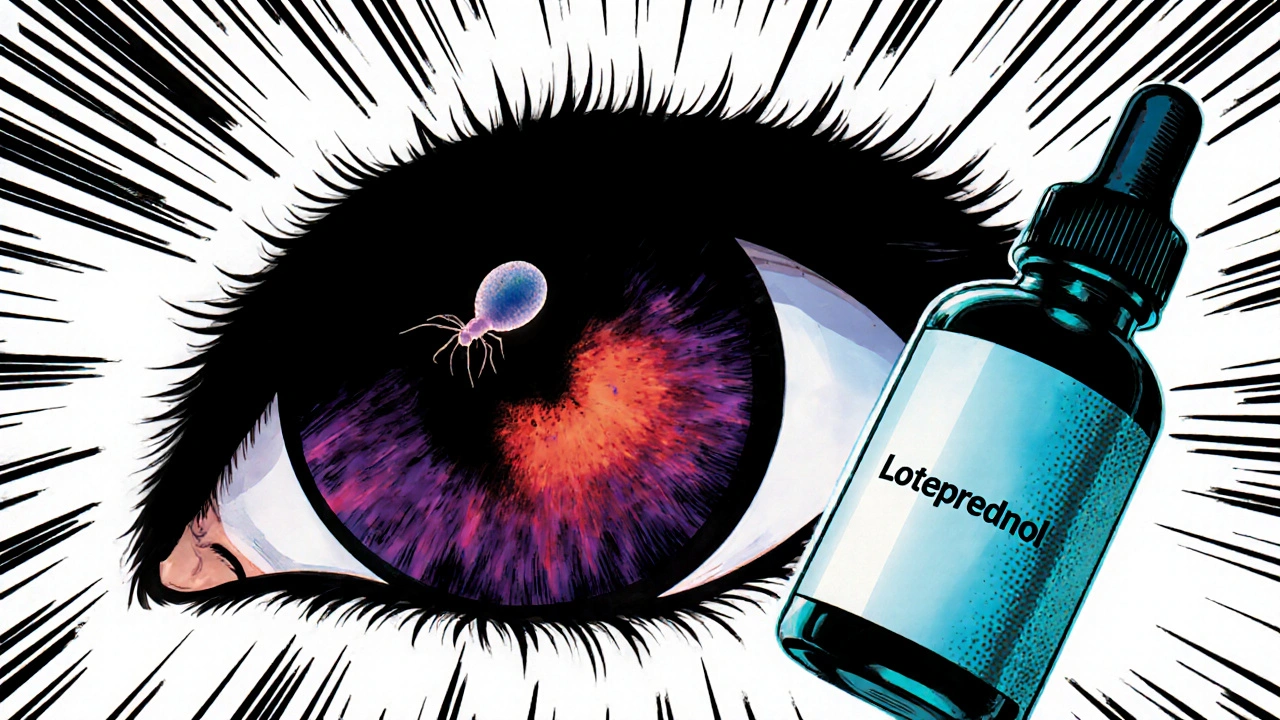
Loteprednol Ocular Toxoplasmosis: What You Need to Know
When dealing with Loteprednol ocular toxoplasmosis, the combination of a soft‑steroid eye drop and a parasitic eye infection, clinicians must balance inflammation control with parasite eradication. Also known as Loteprednol for ocular toxoplasmosis, this approach targets the retinal lesions caused by ocular toxoplasmosis, an infection of the eye’s retina and choroid caused by the Toxoplasma gondii parasite. The steroid component, Loteprednol, a low‑potency corticosteroid formulated as an eye drop to reduce intra‑ocular inflammation without triggering high intra‑ocular pressure, works hand‑in‑hand with antiparasitic therapy, drugs such as pyrimethamine, sulfadiazine, or clindamycin that kill the Toxoplasma organism. Together they form a therapeutic pair that aims to preserve vision while keeping inflammation in check.
Key Treatment Components
In practice, loteprednol ocular toxoplasmosis treatment follows three main steps: diagnose, dampen inflammation, and eliminate the parasite. Diagnosis typically involves a slit‑lamp exam, fundus photography, and sometimes PCR testing of aqueous humor to confirm Toxoplasma DNA. Once confirmed, ophthalmologists prescribe a short course of Loteprednol eye drops, often twice daily for a week, then taper based on retinal edema and patient comfort. Simultaneously, antiparasitic therapy kicks in, usually a 4‑week regimen of pyrimethamine‑sulfadiazine plus folinic acid to offset bone‑marrow suppression. The steroid helps reduce macular swelling, which can otherwise lead to permanent vision loss, while the antiparasitic clears the underlying infection. This dual‑action model reflects a common semantic triple: “Loteprednol ocular toxoplasmosis treatment combines anti‑inflammatory eye drops with antiparasitic medication.” Another useful triple is: “Corticosteroid eye drops require careful intra‑ocular pressure monitoring.” Finally, “Effective antiparasitic therapy influences the speed of lesion resolution.” Patients often wonder about side‑effects. Loteprednol’s low propensity for raising intra‑ocular pressure makes it safer than older steroids like prednisolone, but regular pressure checks remain essential, especially for glaucoma‑prone individuals. Antiparasitic drugs can cause gastrointestinal upset, rash, or rare blood‑cell abnormalities, so routine blood work is recommended during the first two weeks. Adjustments—such as swapping sulfadiazine for clindamycin in sulfa‑allergic patients—are common and illustrate the relationship: “Drug allergy influences choice of antiparasitic therapy.” When managing pediatric cases, dose reductions and close follow‑up are vital, because children may experience more pronounced inflammatory responses. Beyond the core regimen, supportive care can improve outcomes. Nutritional advice (adequate folic acid intake) helps counteract pyrimethamine‑induced folate deficiency. Patients are encouraged to avoid contact lens wear during active inflammation to reduce secondary infection risk. For those with recurrent lesions, prophylactic low‑dose trimethoprim‑sulfamethoxazole taken twice weekly has shown promise in reducing flare‑ups—a strategy that links prophylaxis to long‑term disease control. All these facets—diagnosis, steroid use, antiparasitic choice, monitoring, and supportive measures—create a comprehensive picture that prepares readers for the detailed articles listed below. Below you’ll find practical guides, dosage charts, side‑effect management tips, and case studies that dive deeper into each aspect of managing loteprednol ocular toxoplasmosis.
Loteprednol's Role in Managing Ocular Toxoplasmosis
Learn how loteprednol works, dosing guidelines, safety checks, and evidence for treating ocular toxoplasmosis, with practical tips and a comparison to other steroids.
Categories
- Medications (69)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (8)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)
Popular Articles



