Infection: Causes, Signs, Treatment & Smart Medication Advice
Infections happen when germs—bacteria, viruses, fungi, or parasites—get into your body and start causing harm. Some infections are mild, like a cold; others can be serious, like pneumonia or untreated tuberculosis. Knowing common signs and when to seek help makes a big difference.
Most infections begin with familiar symptoms: fever, pain, redness, swelling, pus, coughing, sore throat, or diarrhea. Watch for sudden high fever, trouble breathing, severe pain, confusion, or if symptoms get worse after a few days. Those are red flags; go to a clinic or hospital.
Common causes and how they differ
Bacterial infections often respond to antibiotics. Examples here include urinary tract infections, strep throat, and some skin infections. Viral infections—like the flu, herpes, or the common cold—need antivirals only in certain cases; many viral illnesses improve with rest and fluids. Fungal infections affect skin, nails, or lungs in some people. Parasites cause things like intestinal worms or malaria.
Knowing the cause matters because treatment differs. For example, aciclovir treats herpes viruses, while antibiotics won’t help a viral infection. Likewise, for TB, drugs like ethambutol are part of long courses prescribed and monitored by doctors. Never try to mix or change these treatments without medical advice.
Treatment, prevention, and smart medicine shopping
Start treatment based on a doctor’s diagnosis whenever possible. If antibiotics are needed, finish the full course even if you feel better early. Stopping early raises the chance of resistant bacteria. For viral problems, ask about specific antivirals if you are high risk or symptoms are severe.
Prevention beats cure: wash hands, stay up to date on vaccines, cook food safely, and avoid close contact when sick. For chronic conditions like diabetes, keeping good control lowers infection risk. Simple steps like covering coughs, using condoms, and cleaning wounds cut chances of catching or spreading germs.
If you buy medicine online, pick reputable pharmacies and verify they require prescriptions for prescription drugs. Our site has reviews and guides about buying medications safely, from antivirals to diabetes drugs. Watch for offers that sound too good—fake or low-quality meds are a real risk.
Antibiotic alternatives and specifics matter for different infections. For instance, nitrofurantoin or fosfomycin can be better choices than amoxicillin for certain UTIs. Talk with your clinician about allergies, pregnancy, and interactions with other drugs you take.
People with weaker immune systems—older adults, very young children, pregnant people, and those on immunosuppressive drugs—need faster care. Tell your clinician about recent travel, animal exposure, or hospital stays; that information narrows down likely causes. When traveling, pack necessary meds, use insect repellent, and avoid risky foods and water. For outbreaks, follow local health advice and get tested quickly to protect yourself and others. Keep vaccine records handy and ask about boosters when due, regularly.
Finally, keep records of past infections and treatments. That history helps clinicians pick the right drug fast. If symptoms return or don’t get better, ask for tests—blood work, cultures, or imaging—to find what’s really going on.
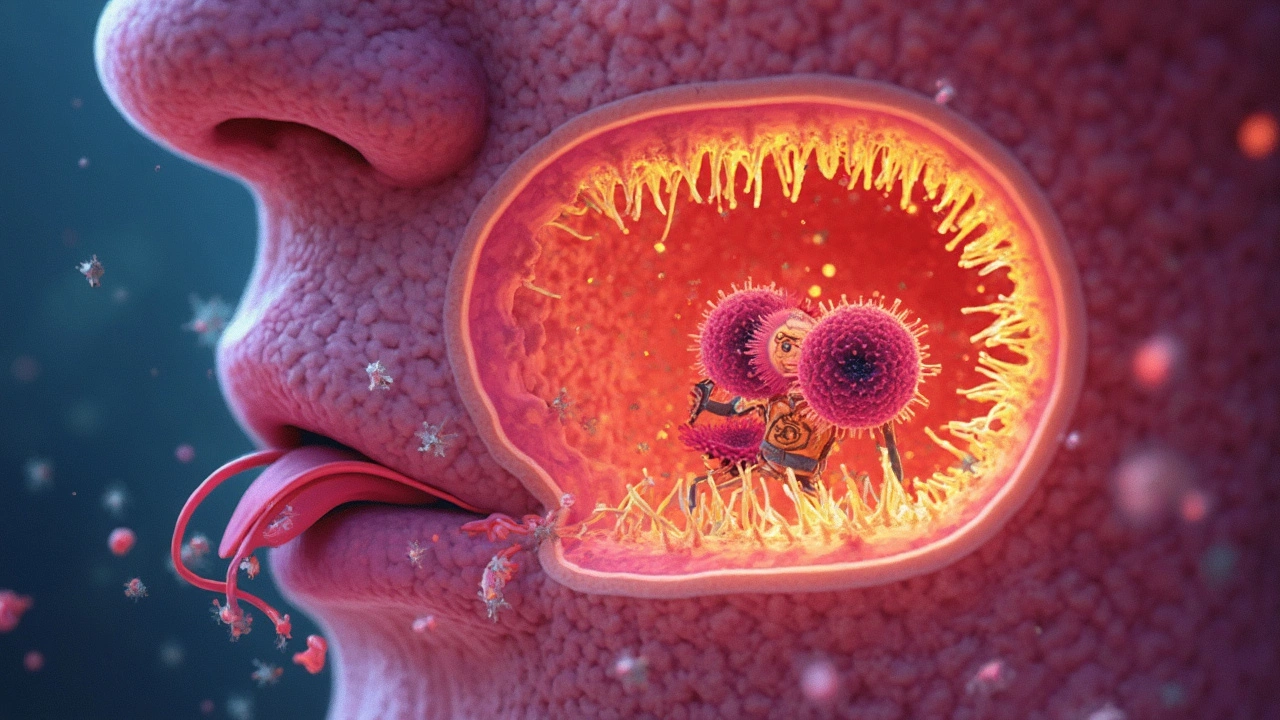
How Pharyngeal Mucous Membranes Guard Against Infection
Think of your pharyngeal mucous membranes as a security team for your throat. They trap and sweep away harmful germs before they sneak into your body. The sticky mucus, cells, and chemicals work together 24/7 to keep you safe. This article breaks down how these membranes do their job, why it matters, and what you can do to keep your throat defenses strong. You'll also get practical tips for daily habits to protect your throat.
Categories
- Medications (72)
- Health and Medicine (62)
- Health and Wellness (38)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)