Hypertension: Practical Steps to Monitor and Manage High Blood Pressure
High blood pressure often shows no symptoms but quietly raises your risk of heart attack, stroke, and kidney problems. Want straightforward actions you can use today? This page gives clear, useful steps for checking your numbers, changing daily habits, and handling medicines without the fluff.
How to measure and track blood pressure correctly
Home monitoring is one of the best ways to know what’s really happening. Use an automatic cuff-style upper-arm monitor — wrist devices are less reliable. Sit quietly for 5 minutes, feet flat, back supported, arm at heart level. Take two readings one minute apart and record both. Do this morning before meds and evening for a few days, then share the log with your clinician.
Know the basic categories: normal is under 120/80 mmHg; Elevated is 120–129 / <80; Stage 1 hypertension is 130–139 / 80–89; Stage 2 is 140/90 or higher. Targets can change based on age and other health issues, so confirm your personal goal with your doctor.
Everyday changes and what medicines do
Small daily changes add up. Cut back on salt — aim for less than 2,300 mg of sodium a day, or lower if your doctor advises. Follow the DASH-style plan: more vegetables, fruit, whole grains, lean protein, and less processed food. Move at least 150 minutes a week of moderate activity (brisk walking works). Lose weight if you’re overweight: even 5% body weight can lower numbers. Limit alcohol, quit smoking, and prioritize sleep.
Many people need medicine to reach targets. Common drug classes are thiazide diuretics, ACE inhibitors, ARBs, calcium channel blockers, and beta-blockers. Each works differently: diuretics help remove extra fluid, ACE inhibitors/ARBs relax vessels, calcium channel blockers reduce vessel constriction, and beta-blockers lower heart workload. Ask your provider which fits your health profile.
Watch for side effects and lab checks. ACE inhibitors can cause cough and affect kidney function and potassium, so doctors often test blood after starting them. Diuretics can change electrolytes. Don’t stop medicines suddenly, especially beta-blockers — that can cause a rebound rise in blood pressure.
Some common things raise blood pressure: NSAID pain relievers, excess alcohol, high salt, and even poor sleep. If your readings suddenly jump above 180/120 mmHg or you have severe chest pain, shortness of breath, vision changes, or confusion, seek emergency care right away.
Tracking your numbers, making steady lifestyle changes, and sticking with prescribed medicines gives you the best chance to control hypertension. Keep a simple BP log, ask clear questions at appointments, and treat this as a long-term habit rather than a one-time fix.

Licorice and Blood Pressure Medications: What You Need to Know
Licorice contains glycyrrhizin, which can raise blood pressure and lower potassium, making blood pressure medications less effective. Learn how it interferes with common drugs like diuretics and digoxin, who's at risk, and what to avoid.
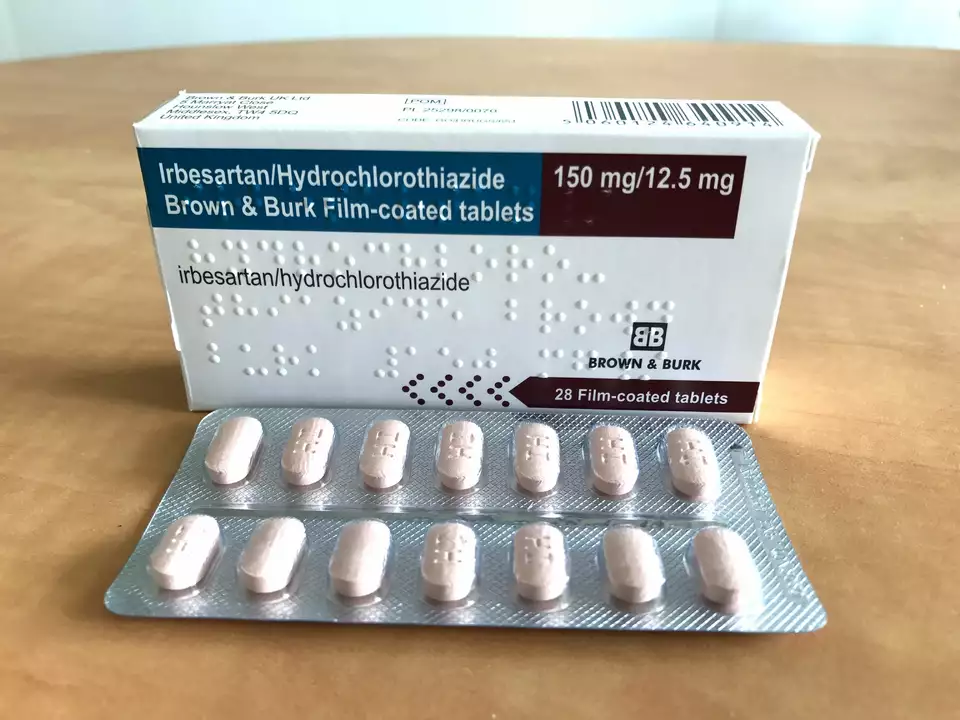
The Effects of Irbesartan Hydrochlorothiazide on Potassium Levels
I recently came across a study on the effects of Irbesartan Hydrochlorothiazide on potassium levels in the body. This medication is commonly used to treat high blood pressure and can significantly impact our potassium levels. The results showed that while some patients experienced a decrease in potassium, others maintained normal levels or even experienced an increase. It's important to monitor potassium levels when taking this medication, as imbalances can lead to health complications. Always consult your doctor for personalized advice and proper dosage adjustments.
Categories
- Medications (70)
- Health and Medicine (60)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)