Herpes simplex virus: what you need to know right now
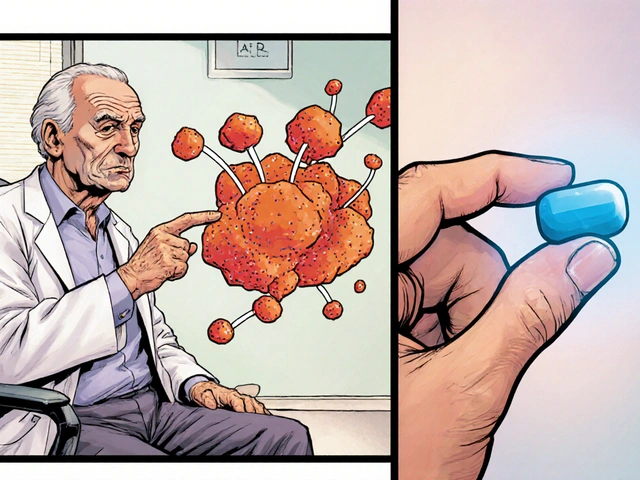
Herpes simplex virus (HSV) causes common skin and mucous membrane infections. There are two main types: HSV-1 usually causes oral cold sores, and HSV-2 most often causes genital herpes. Both can affect either area, and many people carry one of these viruses without obvious symptoms.
How HSV spreads
HSV spreads by direct skin-to-skin contact. That includes kissing, oral sex, genital contact, and sharing items like lip balm during an active cold sore. Important: the virus can shed and infect others even when no sore is visible — this is called asymptomatic shedding. Avoid intimate contact when you or a partner have visible blisters. Condoms lower risk for genital herpes but don’t eliminate it because HSV can infect areas condoms don’t cover.
Primary infection can be more severe than later outbreaks. The first time someone gets infected they might have fever, swollen glands, pain, and multiple lesions. Later recurrences tend to be shorter and less intense.
Treatment and prevention
Antiviral pills shorten outbreaks and reduce transmission. Common medicines your doctor may prescribe are acyclovir, valacyclovir, or famciclovir. Starting treatment as soon as you feel tingling or see a sore helps most. For frequent outbreaks, doctors sometimes recommend daily suppressive therapy to cut the number of recurrences and lower the chance of passing HSV to a partner.
For oral cold sores, over-the-counter options like docosanol can help if used early. Home care eases symptoms: keep the area clean, use cool compresses, avoid touching sores, and take paracetamol/ibuprofen for pain if needed. Use lip balm with SPF to reduce sun-triggered outbreaks.
Preventive steps that work in real life: tell partners you have HSV, avoid sex during active outbreaks, use condoms, consider daily antivirals if you have frequent recurrences, and don’t share personal items when you have a cold sore. Pregnant people with genital herpes should tell their healthcare provider — active genital lesions near delivery can lead to neonatal herpes, which requires immediate medical attention and sometimes a cesarean delivery.
Testing: a swab taken from a fresh sore and tested by PCR gives the clearest answer. Blood tests that detect HSV antibodies (IgG) show past exposure but can’t always pinpoint when or where you were infected. If you’re worried about exposure, talk with your clinician about which test fits your situation.
When to see a doctor: if you have severe or spreading lesions, fever with widespread sores, a first-time outbreak, are pregnant, or have a weakened immune system. Newborns with any suspicious lesion need urgent care.
Living with HSV is manageable. Many people lead full lives with simple precautions, early treatment, and honest communication with partners. If you have questions about symptoms or treatment options, set up a chat with your healthcare provider — they can tailor advice to your situation.

Aciclovir Uses, Side Effects, and Dosage: Your Complete Guide
Discover what Aciclovir does, how it works, when to take it, and what to watch out for. Essential guide for anyone dealing with viral infections.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)