Eating disorders: practical signs, help, and safe treatment options
Ever worry that someone you care about is changing around food, weight, or eating habits? Eating disorders are common and serious, but getting the right help early makes a big difference. This page gives straightforward signs to watch for, what treatment can look like, and how to stay safe if medication or supplements become part of the plan.
Spotting common signs
Eating disorders show up in different ways. Anorexia often means extreme food restriction, intense fear of gaining weight, and dramatic weight loss. Bulimia includes bingeing large amounts of food followed by purging through vomiting, laxatives, or excessive exercise. Binge-eating disorder involves repeated episodes of eating large amounts without purging. Some people develop avoidant/restrictive food intake disorder (ARFID) and avoid foods for sensory or fear-based reasons.
Watch for physical signs like fainting, dizziness, irregular heartbeat, or noticeable dental erosion. Behavioral signs include secretive eating, rigid rules about food, ritualized meals, or sudden avoidance of social meals. Emotional signs can be low self-worth, intense anxiety about body shape, or mood swings. If someone mentions suicidal thoughts or you see signs of severe medical decline, seek emergency care.
Practical steps to get help
Start with a calm, non-judgmental conversation. Say you’re worried and want to support them. Encourage a medical check-up—blood tests, ECG, and weight monitoring can spot dangerous issues early. A registered dietitian with eating-disorder experience can help create a safe meal plan and reduce fear around food.
Therapy is the core treatment. Cognitive-behavioral therapy (CBT) helps with binge and purge behaviors. Family-based treatment (FBT) is often best for teens. Dialectical behavior therapy (DBT) helps with emotion regulation. Medication can help some people—SSRIs are sometimes used to reduce bingeing and treat coexisting anxiety or depression—but meds should only be started under professional care.
If you consider online pharmacies for prescribed medications or supplements, choose licensed sellers. Look for clear contact info, require a prescription, check verified reviews, and avoid prices that seem too good to be true. Never use appetite suppressants or unverified supplements without a clinician’s approval—some products can cause heart rhythm problems or dangerous interactions.
If you’re supporting someone: offer practical help like attending appointments, helping prepare structured meals, and setting gentle boundaries around discussion topics. Avoid blaming or focusing on weight—talk about health and feelings instead.
Recovery often comes in steps. Some people need outpatient therapy, others need medical stabilization or residential programs. Keep expectations realistic: progress can be slow, and setbacks happen. That doesn’t mean treatment isn’t working. Stay patient, keep support consistent, and get professionals involved early.
Want reliable resources or safe medication info? Check our site for articles on nutrition, mental health treatments, and safe online pharmacy tips. If you need immediate help, contact local emergency services or a crisis line—don’t wait.
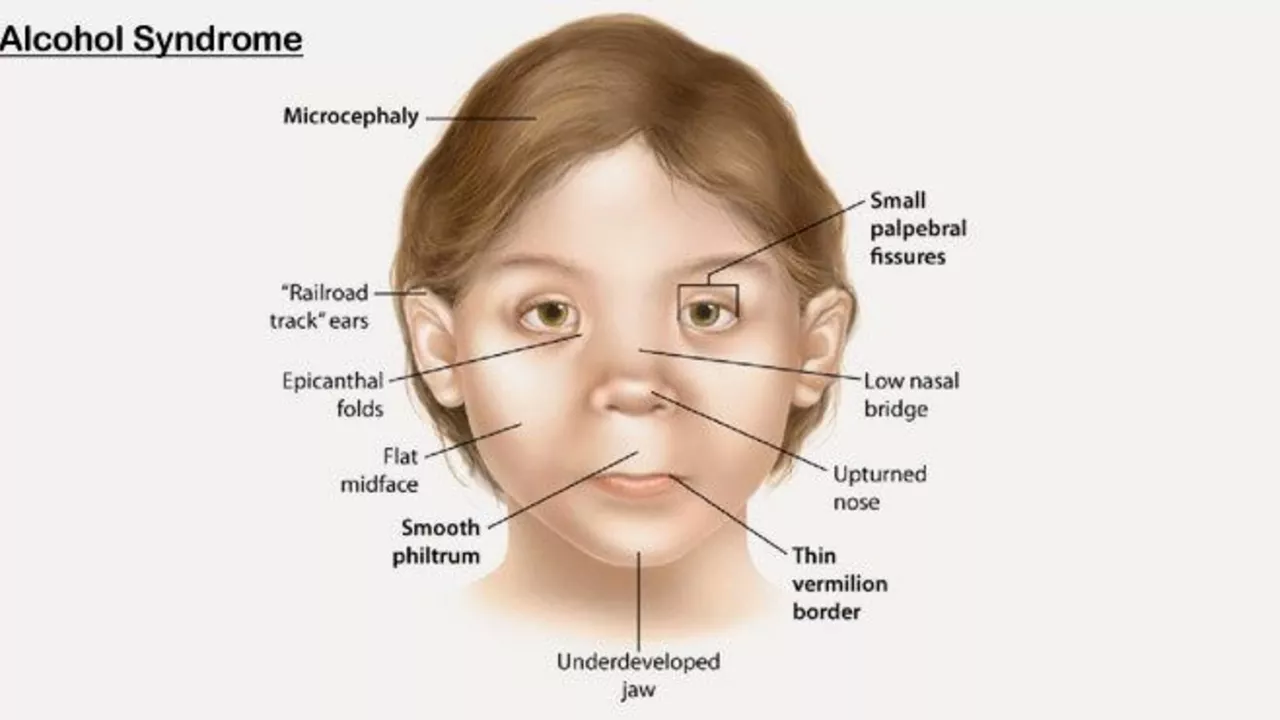
The Connection Between Alcohol Dependence Syndrome and Eating Disorders
In my recent deep dive into health issues, I've uncovered some startling information about the link between Alcohol Dependence Syndrome and Eating Disorders. It's unsettling to know that those struggling with alcohol addiction often also wrestle with abnormal eating behaviors. The dual diagnosis is a vicious cycle, with each disorder feeding the other, making recovery even more challenging. Additionally, it's crucial to understand that both disorders can trigger serious physical and mental health complications. Awareness and understanding of this connection are key for effective treatment and recovery.
Categories
- Medications (70)
- Health and Medicine (61)
- Health and Wellness (36)
- Online Pharmacy Guides (16)
- Nutrition and Supplements (9)
- Parenting and Family (3)
- Environment and Conservation (2)
- healthcare (2)
- prescription savings (1)
Popular Articles



