Pregnancy and Medications: What You Need to Know About Teratogenic Risks and Birth Defects
Pregnancy Medication Safety Checker
Check Medication Safety During Pregnancy
Enter a medication name and select your trimester to see safety information based on current medical guidelines.
When you’re pregnant, every pill, supplement, or over-the-counter remedy feels like a potential gamble. You want to feel better-maybe you have a headache, nausea, or anxiety-but you’re terrified that the very thing helping you could harm your baby. This isn’t just fear; it’s a real, science-backed concern. About 2-3% of all birth defects are linked to medications taken during pregnancy. That number might sound small, but for the families affected, it’s everything.
What Exactly Is a Teratogen?
A teratogen is any substance that can interfere with fetal development and cause birth defects. It’s not just illegal drugs or dangerous chemicals-it includes prescription meds, over-the-counter painkillers, and even some herbal products. The most infamous example is thalidomide. In the late 1950s, this drug was prescribed to pregnant women for morning sickness. By 1961, more than 10,000 babies worldwide were born with missing or shortened limbs. That tragedy changed medicine forever. Today, we know teratogens don’t just cause obvious physical deformities. They can lead to heart defects, brain damage, vision or hearing loss, and even long-term learning disabilities. The timing of exposure matters more than you think. The first 12 weeks of pregnancy-when organs are forming-are the most dangerous window. Between days 15 and 60 after conception, the embryo is especially sensitive. A medication that’s harmless in week 14 could have been devastating in week 6.Medications with Proven Risks
Not all drugs are equally risky. Some have clear, well-documented dangers. Here are a few that doctors strongly advise against during pregnancy:- Warfarin: This blood thinner can cause fetal warfarin syndrome-characterized by a flattened nose, bone problems, eye damage, and developmental delays. The risk is highest in the first trimester, but even later use can lead to bleeding in the baby or brain damage.
- Methotrexate: Used for autoimmune diseases and cancer, this drug blocks folate, a nutrient critical for spinal cord development. Exposure in early pregnancy raises the risk of neural tube defects by 10-20%.
- Carbamazepine: An anti-seizure medication that increases the chance of spina bifida by about 1%. It can also cause bleeding in newborns due to low vitamin K.
- Factor Xa inhibitors (rivaroxaban, apixaban, edoxaban): These newer blood thinners cross the placenta, and there’s no way to reverse their effects if bleeding occurs. No safe dose has been established.
- Cannabis (THC): Even if you think marijuana is "natural," THC crosses the placenta. Studies show a 15-20% higher risk of low birth weight, 10-15% higher risk of preterm birth, and possible long-term effects like attention problems and lower IQ scores in children.
Some medications, like isotretinoin (Accutane) for acne, are so dangerous they come with mandatory pregnancy tests and counseling before prescription. If you’re on any of these, talk to your doctor immediately-do not stop cold turkey without guidance.
The Acetaminophen Controversy
No drug in pregnancy has sparked more debate than acetaminophen (Tylenol). For decades, it was considered the safest option for fever and pain. But recent studies have raised red flags. Some research links long-term, high-dose use during pregnancy to a slightly higher risk of ADHD and autism in children. Here’s the catch: no one has proven acetaminophen causes these conditions. The CDC says the evidence is "suggestive," while the American College of Obstetricians and Gynecologists (ACOG) issued a strong statement in September 2025 saying acetaminophen remains the best and safest choice for pain and fever in pregnancy. Why? Because untreated fever-especially above 101°F-can raise the risk of neural tube defects by 20-30%. So what’s a pregnant person supposed to do? ACOG’s message is clear: the risks of not treating pain or fever are far greater than the theoretical risks of acetaminophen. Use the lowest effective dose for the shortest time. Don’t panic, but don’t take it daily without a reason.
Timing Matters: First, Second, Third Trimester
The effects of medications change depending on when you take them:- First trimester (weeks 1-12): This is when organs form. Exposure here can cause major structural defects-heart, brain, limbs, face.
- Second trimester (weeks 13-26): Major organs are done forming, but the brain and genitals are still developing. Risks shift toward functional problems-like hearing loss, behavior changes, or subtle growth delays.
- Third trimester (weeks 27-birth): The baby’s organs are mostly built, but they’re still maturing. Medications here might cause withdrawal symptoms (like with opioids), low blood sugar, or breathing problems after birth. Some drugs can also trigger early labor.
Even if you took a medication before you knew you were pregnant, don’t panic. Most exposures don’t lead to problems. But do tell your provider right away. They can help you assess the risk based on timing, dosage, and your medical history.
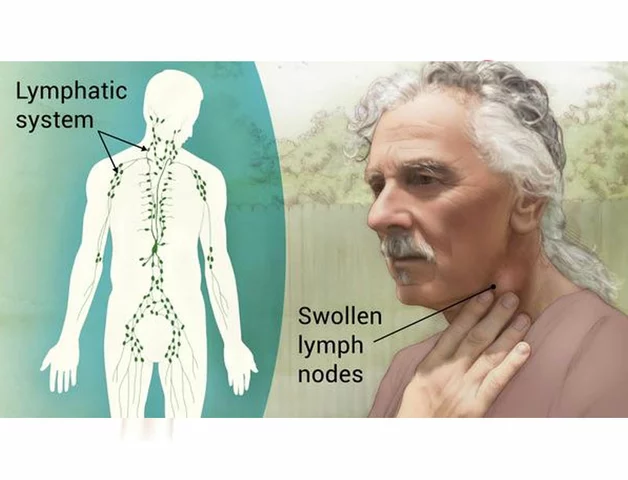
How Medications Actually Affect the Fetus
It’s not just about the drug itself. Five main pathways determine how a medication impacts pregnancy:- No effect: About 60-70% of medications pass through the placenta with no harm to the fetus.
- Direct damage: The drug attacks developing cells-like methotrexate disrupting DNA.
- Indirect harm: A drug lowers your blood pressure so much that less oxygen reaches the baby.
- Placental interference: Some meds block nutrients or oxygen from crossing into the placenta.
- Uterine stimulation: Certain drugs can trigger contractions, leading to preterm birth.
This is why a drug that’s safe for a non-pregnant person might be dangerous during pregnancy. It’s not just about toxicity-it’s about how the body changes during pregnancy and how the baby responds.
What You Should Do Before and During Pregnancy
You don’t have to guess. Here’s how to take control:- Before you get pregnant: Review all your medications with your doctor or pharmacist. If you’re on something risky, like an anti-seizure drug or antidepressant, there may be safer alternatives.
- During pregnancy: Never start, stop, or change a medication without talking to your provider. Even "natural" supplements like St. John’s Wort or high-dose vitamin A can be dangerous.
- Use trusted resources: Don’t rely on Google or Reddit. Use MotherToBaby (a free service run by teratology experts), LactMed (for breastfeeding safety), or the FDA’s pregnancy labeling.
- Ask questions: "Is this necessary?" "Is there a safer option?" "What happens if I don’t take it?" These are valid, important questions.
Here’s something many women don’t realize: about 40-50% of pregnancies are unplanned. If you’re sexually active and not using birth control, assume you could be pregnant. That means avoiding known teratogens like isotretinoin, ACE inhibitors, and high-dose NSAIDs even before you test positive.
The Reality of Missing Data
Here’s the uncomfortable truth: for about 70-80% of medications, we simply don’t have enough data on safety during pregnancy. Why? Because we can’t ethically test drugs on pregnant women in clinical trials. Most of what we know comes from animal studies, accidental exposures, or tracking women who took medications before realizing they were pregnant. That’s why pregnancy registries exist-voluntary programs where women report what they took and how their babies turned out. But only 15-20% of eligible women join them. The FDA is working on using real-world data from millions of electronic health records to fill these gaps, but it’s slow. Until then, the safest approach is this: if you don’t need it, don’t take it. If you do need it, use the lowest dose for the shortest time-and always get professional advice.What About Mental Health Medications?
This is one of the hardest decisions. Untreated depression or anxiety during pregnancy can lead to poor nutrition, preterm birth, low birth weight, and even postpartum depression that affects bonding and infant development. Some antidepressants, like SSRIs (sertraline, citalopram), have been studied more than others. While there’s a small increased risk of heart defects or persistent pulmonary hypertension in newborns, the overall risk remains low. Stopping medication abruptly can trigger relapse-which is often more dangerous than the drug itself. ACOG and the American Psychiatric Association agree: the decision must be individualized. For some women, staying on medication is the safest choice. For others, therapy or lifestyle changes might work better. Don’t let fear silence your needs.Final Takeaway: Balance, Not Fear
Pregnancy isn’t the time to panic about every pill. It’s the time to be informed. Most medications don’t cause birth defects. But some do-and the stakes are high enough that you need to be proactive. The goal isn’t to avoid all drugs. It’s to avoid unnecessary ones. Use what you need, when you need it, at the lowest dose possible. Talk to your provider. Use reliable sources. And remember: untreated illness can be just as dangerous as medication.Can I take Tylenol while pregnant?
Yes, acetaminophen (Tylenol) is currently considered the safest option for pain and fever during pregnancy. The American College of Obstetricians and Gynecologists (ACOG) affirms its use, especially since untreated fever can raise the risk of birth defects by 20-30%. However, use the lowest effective dose for the shortest time. Avoid daily or long-term use without medical advice, as some studies suggest a possible link to developmental issues, though no direct cause has been proven.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most medications don’t cause birth defects, and many exposures-especially early on-have no effect. Tell your provider what you took, when, and how much. They can assess the risk based on the drug, timing, and your medical history. In many cases, the risk is very low or negligible. The key is to avoid repeating the exposure moving forward.
Are herbal supplements safe during pregnancy?
No, not necessarily. Many herbal products are unregulated and lack safety data for pregnancy. High doses of vitamin A, black cohosh, goldenseal, and certain essential oils can be harmful. Even "natural" doesn’t mean safe. Always check with your provider before taking any supplement, tea, or remedy.
Is it safe to take antibiotics while pregnant?
Many antibiotics are safe during pregnancy, including penicillin, amoxicillin, and cephalosporins. Avoid tetracycline (can stain baby’s teeth), sulfonamides (risk of jaundice), and fluoroquinolones (linked to joint problems). Always confirm with your provider-some infections, like urinary tract infections, are more dangerous if left untreated than the antibiotics used to treat them.
Where can I get reliable information about medication safety in pregnancy?
Use trusted sources like MotherToBaby (a free service run by teratology specialists), the FDA’s Pregnancy and Lactation Labeling Rule, and LactMed (for breastfeeding). Avoid relying on Google searches, social media, or anecdotal advice. Your pharmacist is also a valuable resource-they can review your entire medication list and flag potential risks.





shubham seth
November 18, 2025 AT 12:37Yo, this post is a godsend. I was on warfarin for AFib before I got pregnant and nearly had a panic attack every time I had to take it. Turns out my OB had me switch to heparin-no regrets. But honestly, the part about THC scared me shitless. I thought vaping weed was harmless ‘cause it’s ‘natural.’ Turns out my baby’s IQ might’ve taken a hit? Fuck. I’m never touching it again.
Kathryn Ware
November 19, 2025 AT 04:18Thank you SO much for writing this 💗 I was terrified after taking Tylenol for three weeks straight during my first trimester because I had a sinus infection and couldn’t sleep. I read every Reddit thread and almost cried reading the ‘possible link to ADHD’ stuff. But reading ACOG’s stance made me breathe again. I’m 28 weeks now and my baby is kicking like a champ. Use the lowest dose, yes-but don’t let fear paralyze you. Untreated fever is way worse. Also, if you’re on SSRIs, PLEASE talk to your psychiatrist. Stopping cold turkey is a recipe for disaster. You’re not a bad mom for needing meds. You’re a smart one for asking questions 🌸
kora ortiz
November 19, 2025 AT 16:08Stop panicking. If you’re reading this you’re already doing better than 90% of pregnant people. Don’t Google. Don’t scroll. Talk to your provider. Acetaminophen is safe. SSRIs are often safer than depression. Herbal tea? Probably not. Unregulated supplements? Absolutely not. You don’t need to be perfect. You need to be informed. And you’re already here. That’s enough.
Jeremy Hernandez
November 21, 2025 AT 06:57LMAO look at this corporate-approved propaganda. They say acetaminophen is safe but won’t tell you about the 2023 JAMA study that showed a 30% spike in autism spectrum diagnoses in kids exposed to daily Tylenol. And don’t get me started on the FDA-they’re owned by Big Pharma. They banned thalidomide but still let you take SSRIs? That’s just a different kind of poison. They want you scared but not scared enough to question the system. Wake up. Your baby’s brain is a lab rat.
Tarryne Rolle
November 22, 2025 AT 22:24It’s not about whether the drug is safe-it’s about whether we should be taking drugs at all during pregnancy. Nature didn’t intend for us to chemically alter our fetal development. We’ve become a society that medicates every discomfort instead of resting, eating well, or sitting with discomfort. The real teratogen is our addiction to control. Let the body do its work. Let the fetus develop without synthetic interference. Is a headache really worth risking a soul’s blueprint?
Kyle Swatt
November 23, 2025 AT 06:53Man I just want to say I’ve been through this twice. First time I was a mess-terrified of every cough drop. Second time I read this exact post and just chilled. The truth is most meds don’t do shit. The placenta isn’t some flimsy sieve-it’s a smart filter. But yeah, warfarin? Avoid. Methotrexate? Hell no. Tylenol? Fine. But if you’re on antidepressants and you’re crying in the shower every day? That’s the real threat. Your mental health isn’t a luxury. It’s part of your baby’s foundation. Don’t let fear make you a martyr. Be smart. Be kind to yourself.
Deb McLachlin
November 23, 2025 AT 21:59This is an exceptionally well-researched and clinically grounded summary. The distinction between structural and functional teratogenic effects based on gestational timing is particularly valuable. I appreciate the emphasis on evidence-based resources such as MotherToBaby and LactMed, as public misinformation remains pervasive. The acknowledgment of data gaps is commendable-epidemiological studies on medication exposure remain observational and subject to confounding variables. A multidisciplinary approach involving obstetricians, pharmacists, and mental health professionals is essential for optimal decision-making.
saurabh lamba
November 25, 2025 AT 13:28bro why are we even talking about this like it's a science thing? just don't take shit. period. if you got a headache, lie down. if you're anxious, breathe. if you're sick, let your body fight it. pills are for weak people. i took zero meds during my wife's pregnancy and our kid is 7ft tall and speaks 5 languages. just saying.
Kiran Mandavkar
November 26, 2025 AT 20:13You people are so naive. You think the FDA cares about your baby? They care about liability and market share. That ‘safe’ acetaminophen? It’s in every damn product from cold medicine to baby drops. And the studies linking it to neurodevelopmental issues? Buried under layers of industry-funded ‘reanalysis.’ You’re being manipulated into trusting a system that profits from your fear and your compliance. Wake up. The only truly safe medication is none at all. And if you’re still taking Tylenol, you’re part of the problem.
Eric Healy
November 27, 2025 AT 10:29so i took ibuprofen once at 6 weeks and now my kid has 3 fingers on one hand jk but like… if you’re gonna take something you better be damn sure. i had a friend whose baby had a cleft palate and turns out she was taking that migraine med everyone swears is fine. don’t be her.
Shannon Hale
November 28, 2025 AT 07:25THEY DON’T WANT YOU TO KNOW THIS BUT CARBAMAZEPINE IS A SLEEPING TIME BOMB FOR YOUR BABY’S SPINAL CORD. I WAS ON IT FOR SEIZURES AND MY DAUGHTER HAD SPINA BIFIDA. I DIDN’T KNOW. NO ONE TOLD ME. NOW I’M A MOTHER WHO CAN’T HOLD HER BABY WITHOUT CRYING. IF YOU’RE ON ANY ANTI-SEIZURE DRUG-STOP READING AND CALL YOUR DOCTOR. RIGHT NOW. I’M NOT KIDDING. I’M NOT DRAMATIC. I’M A MOTHER WHO LOST TIME.
Holli Yancey
November 29, 2025 AT 10:04I just wanted to say thank you to everyone who’s shared their stories here. It’s easy to feel alone in this. I was on sertraline through both pregnancies and felt guilty every single day-even though my doctors said it was the best choice. My kids are 3 and 5 now, thriving, happy, smart. I didn’t take any extra meds. I didn’t need to. But I’m so glad I didn’t quit cold turkey out of fear. Sometimes the bravest thing you can do is choose yourself so you can be there for your child.